Life, Cancer, Etc.
Life, Cancer, Etc.
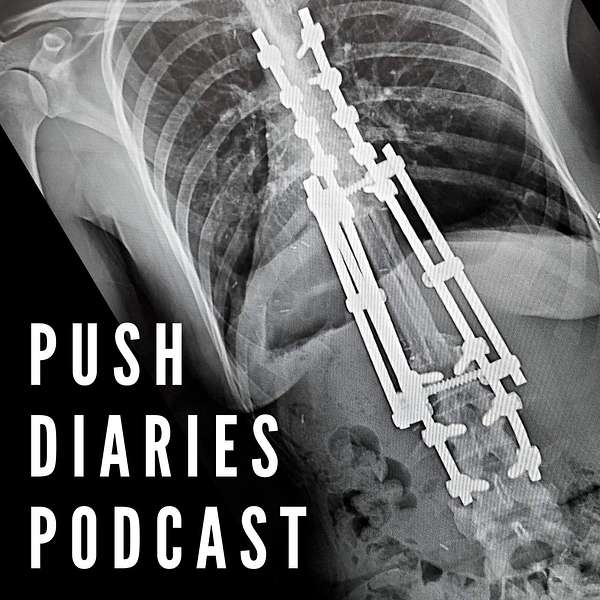
Fellow Sarcoma Survivor Tess Pfohl of "Push Diaries Podcast"
Tess Pfohl is an amazing example of resilience, adaptability, and hope. She's a fellow sarcoma survivor who decided -- at age 24 -- to get a lifesaving cancer surgery that she knew would leave her paralyzed. Tess's positive outlook and the frank way she shares her story are pretty awe-inspiring, and we talked for 2 hours! After you listen to our conversation, you can find Push Diaries Podcast and learn more about Tess here: https://www.pushdiariespodcast.com/
Photo © Tess Pfohl and Push Diaries Podcast
You can also find some episodes on our YouTube channel: https://www.youtube.com/c/LifeCancerEtc
Patreon: https://patreon.com/lifecanceretc?utm_medium=unknown&utm_source=join_link&utm_campaign=creatorshare_creator&utm_content=copyLink
NOTE: I am not a medical professional. Everyone on the "Life, Cancer, Etc." podcast is sharing their own experiences, not giving medical advice.
All content not otherwise specified ©2025 Heidi Bragg and Life, Cancer, Etc. All rights reserved.
I'm Heidi Bragg, and this is Life, Cancer, Etc. My goal with this podcast is to connect you with stories and resources that help you feel happier, more resilient, and less stressed, especially when you're going through hard times. Today I'm talking with Tess Full, and Tess is a fellow sarcoma cancer survivor. She had an osteosarcoma, which is sarcoma in the bone. I had a soft tissue sarcoma, and they're similar and different at the same time. It was so weird that I saw your thing. I found Tess through a group I was in on Facebook, and she was just talking a little bit about her story and having started... It was almost exactly a year, right?
SPEAKER_03:Yeah, yes. Actually, February 20th is the first day my very first episode ever came out. And Heidi, when was your first podcast? When did you first start?
SPEAKER_01:It was the beginning of November in just last year, like I just started. Okay.
SPEAKER_03:So cool. It's so exciting, though. And before you know it, it's going to be November and it's going to be a year for you, too. And I keep telling people, I think it's incredible that, you know, as messed up as 2020 was, right, with the pandemic and the uncertainty and fear surrounding it, I think it's pretty cool that you and I were brave enough to, I don't know, put our nose to the grindstone and start something that we thought could bring hope to other people. So, yes. Heidi saw my post on a group we both follow, and I just thought, you know what? All these people in this group, we've all lived through something, right? Especially after just the crazy year we had with COVID and it being another political year that was very polar opposite. Yeah. I think a lot of people too feel pretty lonely and pretty isolated during something like that, not to mention if you have had cancer. So
SPEAKER_01:have you... Okay, first... Let's talk about your story. And then I want to talk about what's going on now. So do you mind telling your story first? And Tess and I are going to cross post this on each other's podcast. Hers is called Push Diaries Podcast. And it's all about people who've pushed through hard stuff.
SPEAKER_03:Yes. And Heidi's is called Life Cancer ETC. So et cetera. And she is kind of doing the same thing as far as trying to spread hope and awareness and education to people that haven't ever been through this before. Obviously, Cancer is something that Heidi and I never had to deal with on such a personal level as it being an issue that we had to go through on our own. And so, yeah, this is just so cool. I'm excited for people to hear your story and I'm excited for your listeners to hear mine. And it's going to be really fun to collaborate with you, you know, over the coming months and years. So thank you. Absolutely. Reaching out and being brave because that's not always easy to do. Yeah.
SPEAKER_01:What the heck? I mean, it doesn't, it doesn't hurt anything. And if somebody says no, that's okay. Cause that's their experience. Yep. Okay. So tell us, tell us, um, kind of a little bit about you and then your cancer story.
SPEAKER_03:Okay. So I grew up in a town of like I think it was 2,000 to 4,000 people. And then by the time I graduated high school in 2007, I think we had 6,000 people. Mayo Clinic, for those listeners of yours that are familiar with Minnesota, the Mayo Clinic is a huge, world-renowned, certainly one of the best in the United States for really any health care. There was actually a PBS documentary about it. I think about two years ago, and it was called like The Miracle in the Cornfield or something like that. And it talked about how kind of bizarre it was that Mayo Clinic ever just sprouted there, but the Mayo brothers grew up there. I guess their dad was a surgeon and he taught his boys really everything they needed to know about the science around healthcare and surgery. And it just grew into this enormous thing. And so in high school and growing up, I was a really easygoing kid. I'm the first born of three children. My parents are still together. Although it has been difficult at times, our family has managed to, you know, get through, you know, my sister's five years older than me, my brother's three years older than me, and then I'm the youngest. And so I love to do high kick dance. I loved tennis. Oh, hang on. to
SPEAKER_01:run. Like Irish dance?
SPEAKER_03:Well, it's funny you say that. Not Irish dancing, but I'm sure we took some skills from the Irish dancing folks. But no, like high kick, like dance line. Oh, like
SPEAKER_01:drill team. Yeah, I did drill team in high
SPEAKER_03:school. Yeah, kind of like, what are the dancers called at this time?
SPEAKER_01:The
SPEAKER_03:Rockettes. The Rockettes. I like that. Yeah. So it would be like a two minute song and we would come up with choreography, you know, to the, to the eight.
SPEAKER_01:No, I totally. Yeah. I know exactly what you're talking about.
SPEAKER_03:And so I loved that. Like I loved team sports, right? Like that was just fun for me. And then I wasn't really good at like basketball or volleyball. Like I liked it, but I didn't feel like I was very good at it. So dance was a way I could, be on a team, right? But have it be a little bit more, I don't know, unison and less competitive amongst all the dancers. I mean, sure, there were people that were very competitive, but I truly, I wasn't, I wanted our team to succeed as a whole and not just be the best dancer. Does that make sense?
SPEAKER_01:Oh yeah. Well, and, and, and when you're on a drill team or a dance team or dance, what do you call it? What did you call it? Like a dance line. Yeah. Okay. I don't know if it's a big deal in Minnesota. but it's a big deal in Texas because I went to high school in Texas. Yeah. Holy moly.
SPEAKER_03:Yeah. It's a big deal.
SPEAKER_01:And did you have different outfits for the different, like you had three or four, you rotated through and then you do another one at the pep rallies. Yeah. Like another routine. Yeah.
SPEAKER_03:See, that's just so fun too. Yeah. Well, like they say in Texas, go big or not at all or whatever they say. Yeah. So anyway, I had a really normal routine. upbringing. I mean, truly we didn't have all the money we ever needed and we didn't have, I mean, we did, I had what I needed, excuse me. I'm just saying we didn't live in like extreme, um, you know, luxury. Yeah. Of resources. But, um, I, um, finished high school and I went on to college and I thought for sure I wanted to be a nurse and I went into college and I'm just thinking like, gosh, this is not as easy as I thought, like chemistry and biology and, and stuff like that was just very confusing for me and hard for me to get excited about. And I guess I realized the, the more I studied, the more I really thought social work or sociology would be a better fit for me. Um, I thought maybe one day I could be a counselor or a psychologist or, you know, a lead social worker in a nursing home or in a hospice department or something like that. And so I started to go to school for that. And I finally finished with a five-year degree instead of four years because I really hit that nursing stuff hard and then realized like, man, I got to switch that up. And it's like, Heidi, did you know when you went to school exactly what you wanted to be or did you change?
SPEAKER_01:No, no, no, no, no, no. I went in as a communications major and then I changed to business, which is interesting because I do marketing now. Okay. But then... The business program was very, very... I went to Brigham Young in Provo in Utah. And it was very, very competitive. And it was very... Let's just say it was very male at the time.
SPEAKER_03:Yeah.
SPEAKER_01:And I had people say to me, why do you want to take my spot? Because you're just going to be barefoot and pregnant. And I was like... What century are we living in? Yeah. Doofus. Yeah. Anyway.
SPEAKER_03:Well, Brigham Young, that's a huge school. I've heard of that.
SPEAKER_01:Yeah. I think we had like 25,000 at the time and they have more now. But anyway, so they were, I had taken some econ classes and I really liked them. And they were just building the economics program at BYU. And so I switched to econ and there were, I was one of three women in the program at the time. I got mentored to death. there were great professors. And I mean, professors from big powerhouse econ schools, like, you know, Northwestern and Berkeley and Yale. And I mean, Princeton, really good people. So that's what I graduated in, but no, I did not know. And it did take me five years because when you, cause I was paying for school myself and earning money in the summers. And when you're doing that and you switch majors, it comes back to bite you.
SPEAKER_03:Oh yeah. Yeah. Yeah. Well, and it's funny, like you said, now you're kind of, even with your podcasting stuff, it's like you're kind of right back in that realm, you know? Yeah. Like talking to people, having conversations, there's bound to be a business aspect, right? How much time are you spending? And maybe one day we can get sponsors. How cool would that be?
SPEAKER_01:I think that's like, I'm like the little league level that would probably be like more like professional, but you know, someday that could be a thing. I don't even know.
SPEAKER_03:Yeah. Who knows? I mean, I think it's really wonderful. These podcasts about hope, because like you said, there's always stuff that we can encourage each other with. Right. And I, I know you're, you have a couple or a few years on me, Heidi, but you know, I'm, I'm 32. I'm saying that with a question. Um, I was born in 89. So I guess I'm turning 32 in March. Okay.
SPEAKER_01:I'll be 53 in April.
SPEAKER_03:Yeah. And so as you know, I'm sure as you were a parent and stuff too, you learn things about life and you go through seasons yourself where you're like, whoa, I didn't realize that people could feel this way. And how can I better help people that are going to feel this way later on? And I know I've been kind of forced to to maybe grow up or experience health and life or death sooner than a lot of people. I know you have too. And so it really is amazing how different it makes us because I feel like Tess was very naive back even when I was done with school. I thought like, oh, I've got my degree now. I'm going to go do this, that, and the other thing. And I had no idea what really God had for me. had planned for my life and the trials that I would go through. And, and I don't say that because I'm mad at God. I just literally, I had no stinking idea. I was so naive. And again, I bet you can be like, yeah, me too. I had no idea. Oh, I had my plan.
SPEAKER_01:And I think a lot of times God's like, that is so good. I'm so glad you made those plans. I appreciate the initiative you took. Okay. Now we're going to not do any of that. So we're going to go over here. And, and, and I think, um, I think coming to be okay with that and coming to be okay with uncertainty, which I hate, is something I've learned more deeply through these cancer experiences over the last seven years.
SPEAKER_03:Absolutely. Yeah. It's so hard to put it into words, but really being even just in the hospital and seeing the way these nurses work and It's just like, wow, I had no idea. But you're right. These experiences really have shaped us and allowed us to be, I don't know, more emotionally connected to people around us. I feel that way. I think so. More sympathetic to what people are going through. And I think it's ultimately going to make me be a better person, as you do. It's almost like you have an introspection that you never had before.
SPEAKER_01:Until you're... I mean, there are some people, I think it's, I've always been relatively introspective, but I never realized the level it could get to with this. And I was, okay, so when were you first diagnosed? Like, how old were you?
SPEAKER_03:So I... I finished my college and then I started working as a social worker.
SPEAKER_01:Oh,
SPEAKER_03:okay, cool. Yes. And I, so I got the job that I didn't think I would get. Honestly, had I stayed at that job for another year, I would have gone back to my master, gone back and gotten my master's and I'd probably still be there today. But they just wanted, they wanted a master's level social worker for this job. And I thought, you know what? One thing that cancer taught me too is like, I always have hope and I had hope before cancer too, which some days I think is what got me through it. But there's also people that have all the hope in the world and don't make it through to the other side. But so I was diagnosed in 2014 and I started working in hospice like in February and And I worked all of February, all of March, all of April. And by like May 6th, I was at the Mayo Clinic.
SPEAKER_01:So what triggered it for you? Like, how did you know?
SPEAKER_03:Yeah, so I started having really bad back pain. It felt sort of like a menstrual cramp for those ladies that are listening to our podcasts. And it really did. It just felt like a dull backache. It kind of maybe was... You know, on both sides, really low, like almost right above my kind of right above my lower back. It just hurt really bad deep in the sides of my spine there. And I was I was absolutely in love with my job. just pouring my heart and soul into it. You know, I was living in a really rundown apartment, but I was going to save up my money and I was going to plan for my future. And I was going to move into Alexandria from Glenwood as soon as I got enough money to pay for, you know, the shorter commute and the nicer apartment. And, you know, every day my back pain just got a little bit worse and a little bit worse. And like I said, I started in February and Um, it just slowly got worse. So like by the end of February, I was like, okay, this is weird. This continues for say another two weeks and isn't getting better. I'm going to go see my, I'm going to go get a doctor. Cause I didn't have a doctor where I was working newly. Um, where I was living was in Cannon Falls, uh, Minnesota, which is about an hour South of the cities there in central Minnesota. And Knute Nelson was like, three and a half or four hours north of where I used to live. So I moved up there, got this apartment. Like I said, my back pain did not get better. So I reached out to the doctors up there in Alexandria and I found a doctor at a clinic and he had a good, you know, He had good reviews and I'm sure I heard about him through people at work and they just said, you know, go to any clinic. It should be fine. You know, I was a healthy, young 24 year old girl who was going on, yeah, jogs with my dog, you know, after work. And I had two cats at home and, you know, my version of a fun, relaxing evening would be like going to the co-op and getting fresh veggies and packing my lunch for Monday and, you know, packing the night before and taking a bath and just watching some TV, you know, like just very normal life. Yeah. Very easy going normal life. But I was so on fire for what I was doing at hospice. Like I felt like God 100% put me in that job. And what I came to realize Heidi is like, God was preparing me for my own facing of life and death. And I had no idea. Um, You know, what are your wishes when you could be on your deathbed in the next weeks or months? What are your wishes if you need IVs or you need a feeding tube? You know, these are really tough conversations to have. And I also knew that as a social worker with my degree, like, there's such a vast... and diverse population of people out there that are going through death that might have a supportive family or might not, might have a job or might not, might have no idea of what it would be like to face cancer or not, you know? And so- We
SPEAKER_01:went through, I lost my sister about almost 30 years ago to a brain tumor. And my dad, it's been five, six years, I think now.
UNKNOWN:Yeah.
SPEAKER_01:to a very fast-moving cancer. He got diagnosed and then died 10 days later. He had been very healthy. So we had hospice. Yeah. I also lost a dear, dear friend to glioblastoma in between those two.
SPEAKER_03:How many
SPEAKER_01:siblings do you have, Heidi? I have six siblings, five living. Okay. But what I was going to say is the hospice... The hospice... the whole hospice program from the social workers to the people who would come and give the caretakers massage because it's a lot of work caring for someone and lifting and moving and just having someone manage the meds. I mean, just all the different pieces that hospice brings in helps make it so that you can be present with your loved one and have somebody else help prompt you for the things you need to decide, take care of the things that you don't need to worry about, et cetera. I can't speak highly enough. So I just want to say kudos to you because I just think hospice is an amazing program.
SPEAKER_03:Yeah. And I totally agree with everything you said. It's so true. And gosh, you as a young woman, I mean, 30 years ago when your sister passed away, even like, I'm sure your family had no idea what on earth, you know, the next days and months were going to be like for you. And I'm so glad to hear that hospice has been, you know, someone in your corner after losing your dad too. That's just, death is so hard for the people that we leave behind. And I, Any little bit helps. I mean, like you said, just knowing what to do with medication and when to give it. It's almost like having
SPEAKER_01:a tour guide or an escort through those very, very difficult things. And I think, I will say this, having had hospice when Mindy died, my sister died, made it so that 25 years later when dad was... And my brother's an ER physician. I mean... But when he was able to get there, he wanted to be there as a kid, as my father's son, not as a medical professional. And so having had that experience with my sister, it was much easier to call in hospice as soon as we knew dad was going downhill really, really quickly and would not be with us very long.
SPEAKER_03:Yeah. Yeah. Yeah, gosh, that must have been so hard. Now, Heidi, I apologize if I'm jumping around, but... Oh, no, you're fine. What do you do for work right now? I
SPEAKER_01:do marketing and organizational health and writing and editing. Yeah. My title is like Senior Marketing Strategist and Editor-in-Chief, and I work for an engineering and manufacturing company that's in Oregon.
SPEAKER_03:Very cool. Very, very cool. But you're living where? In Florida. Okay. That's so fun. So cool. And all your kiddos, are they off to college?
SPEAKER_01:We have one left at home. He's 16 and he's at a collegiate high school. So he's getting his high school diploma and his associates in May, which is awesome.
SPEAKER_03:Yes. Very cool. Well, that's very exciting.
SPEAKER_01:The others are in our daughter who just went to college. This is her first year. She's at BYU, Idaho. We have a son in Eugene who works for the same company I do. And our oldest son is in Payson, Utah. He's an urban planner.
SPEAKER_03:Okay. Okay. Okay. So kind of rewinding, that horrible pain turned into, I remember vividly, One day I was swimming in a pool. at Knute Nelson, we have a older adult facility that's like apartments with, I think, some, you know, room and board and they make like one meal a day. And so,
SPEAKER_01:you know. Wait, so Knute Nelson, is that a facility or a town?
SPEAKER_03:It's a facility. So they have like a hospice agency. They have a nursing home. We have a rehab department. Assisted living. Assisted living, yep. Okay, gotcha. So they had this pool in this assisted living building and I was swimming back and forth doing laps And I think I was in there by myself and the way the water took gravity off of my body just enough made the pressure in my spinal cord or something just weird enough. And it's like, you know, when you sit up too fast and you just see black stars and your vision slowly goes away, but you're completely conscious. That happened to me when I was in the middle of the pool. And I, and I, I think now I had just started to realize when I would do certain leg motions, if I'd kick my heel too far back and up, it would almost make me feel weak or that leg was fatigued, but it was coming from my spine. It was just very odd, things like that, where I was like, oh my gosh, what if I pass out while I'm swimming in the deep end? I'm just having all these... And so I kept going back to this doctor that I finally got in to see. And I said, my pain isn't getting better all day at work. You know, thank God I love my job because I don't know how I'm doing this when I'm getting three hours of sleep a night. I would get home. Go on a run, eat my dinner, get in the bath, pack my lunch for tomorrow and then lay down. And it was like nine o'clock and I just knew like I need to be laying down by nine o'clock because my alarm is going to go off at five thirty or six o'clock and I need to have had my rest. And I know I'm not going to sleep well because I didn't the night before. And so
SPEAKER_01:just because of the pain.
SPEAKER_03:Yes. And just the discomfort. It's like I would lay on my back and that same achy feeling would just be a little bit more intense. So then I lay onto my side and then I'd lay kind of over my side, like half on my stomach, half on my, you know, laying on my stomach, half on my side. And I remember I would not sleep more than three hours. or two hours and I would wake up from the pain and the discomfort. And so I'd go to bed at nine, watch a show till 10, fall asleep from like 10 to midnight or 10 to one. And then at midnight or one, I would get out of my bed, go fill up my bathtub with hot, hot water. And I'd lay in there. And sometimes I'd go back to bed by three and I'd be back into the bathtub at five or just getting relief before my day again. I mean, I do not. There were days I slept on my floor. There were days I blew up an air mattress and slept on that. Because you just couldn't get comfortable. I couldn't get comfortable. And in fact, I just had enough money after these three months of working in hospice to go buy myself a really nice mattress. So you know, my dad was like, Tess, is it because you're just sleeping on your floor and because you're sleeping on your air mattress and you've had all these big changes? And I'm like, I mean, it could be, but I just really don't think that's what's causing this pain. And so went into the doctor, told him about the sensations, told him about how I just can't get comfortable. And he's telling me like, you know what, maybe you just have a like a weak core or a weak midsection, like I think we should just order some physical therapy, get your abs back into it, get your, get the sides of your, you know, abdominal cavity working out again. We'll get your lats really strong in your back. And I'm just thinking like, okay, like I have good health insurance. Go ahead and order those physical therapy visits. But gosh, Heidi, I knew that something wasn't right. And, um, my, um,
SPEAKER_01:But no imaging. I just find that really odd.
SPEAKER_03:So he did do an x-ray, which with a soft tissue tumor, as you know, it doesn't show up on an x-ray. And the early stages of an osteosarcoma bone cancer, they don't show up on x-rays either because they're active on soft tissue. I
SPEAKER_01:did not know that.
SPEAKER_03:And so, yeah, we did an x-ray, didn't show up. My vertebrae looked 100% normal. And I had asked him, I even remember saying like, Dr. Paul, like tell me if you think Imaging could be beneficial for like an MRI or a CT. I said, let's do it. Like I want to know what's going on. And so we kind of came to agreement that if, and say two, three weeks, it wasn't getting better, he would order that imaging. And sure enough, over like a two week time span. Now I'm not just noticing weakness in my legs, but I'm like falling down stairs. I'd get to the edge of my stairway. I lived up like 30 stairs. There was no elevator. Oh, Um, had gotten down all the steps and I had to think about every step I was taking. I mean, literally it was like my brain was telling my feet to, to move and they wouldn't, I mean, you know, as a walking person, that's not something you have to think about. Right.
SPEAKER_01:Right.
SPEAKER_03:So when you're telling your feet to do that and it's just lights out down there, it's like, this is terrifying. And so, um, Finally, I think it took me falling a couple times at work. I remember I was leaning over a gentleman putting a cold washcloth on his forehead. He was probably six hours from leaving this earth, and I couldn't balance on my left leg just to lean. And I fell, and I caught myself, and it was no big deal. I didn't offend the guy. But I literally landed... over him. And, and I put my elbow in the bed and like push myself up and was just like, what the heck is that? Yeah. This is just so bizarre. That is not normal. So I finally went back in there. I called my mom. She, she's been a nurse for 30 years at the time. And I just told her, I said, mom, something's not right. Like, you know, she was the one that I would call at 1230 in the morning, like crying, saying, I don't know what's going on. I didn't, collar crying every night, but there were nights I was just exhausted. I didn't know what was going on. I'm trying to like go running every day and doing all these ab workouts and it was nothing. And so I'm sorry, I could go on and on about this, but it was just so devastating to lose my physical ability over those, those, you
SPEAKER_01:know, and the not knowing the not
SPEAKER_03:knowing is
SPEAKER_01:what just
SPEAKER_03:was just so bizarre.
SPEAKER_01:Yeah.
SPEAKER_03:And so finally he, he bent and he did the MRI for me and I knew something was wrong he was actually doing like thoracic to my lumbar spine and or because it goes cervical thoracic lumbar, right? Yeah. And then synovial. And so he was doing like my mid back down. He wanted to see what was bothering me in my mid back. Cause I was having my pain there. Right. And when you start to talk about like nerves that affect your legs and stuff like that, those are usually a little bit lower nerves. Well, finally the week he ordered the scans, I started to develop this numbness to the left of my belly button. It's like, It's like my whole left half of my body. So like below my breast, next to my belly button, then all the way down into my groin and to the left. And then it started going down my leg and into my thigh bone and into like, what is that joint everybody has issues with that cause numbness in their leg? I'm sciatic. Yes. So it was just very bizarre. And then one day at work, I'm thinking like, Oh my gosh, Heidi, it was like 1.30 and I hadn't gone to the bathroom at all since the morning. And that's not normal for me. Like usually I would empty my bladder before lunch or I just thought like, oh my gosh, I don't even have the sensation to pee. I'm looking at my coffee thinking, no, I drank a whole coffee today and I drank half my water bottle. And that's when I started getting more and more concerned, but I knew I had a MRI coming up. So I held out and I waited and my MRI came up and I'm laying in the machine. And so they're doing that scan of my mid to lower back. And we were probably only 15 minutes into the MRI. And you know, that takes a good hour sometimes for them to go through every little organ and every little bone and they stopped it after 20 minutes they first told me okay this scan could be about 40 minutes we're going to do a couple right after one another so just know that it'll be a while you can close your eye right and try to relax and they stopped it after 20 minutes and then moved the machine up and did it from like my neck all the way down and I thought oh boy this can't be good and we found something that they are looking at extensively now and so That was really scary. And then so I had that done on on a Saturday and the techs did call me, I think, after I got home and they said, we would like to see you right away on Monday. So my mom was able to take Monday off work and stay with me for my results. And so we went back in there. And I remember when we were waiting in the waiting room to go in just from a couple of weeks ago when, you know, things were just uncomfortable. Um, but I could still sit in my chair and work and lean on a heating pad or lean on an ice pack. I remember like I would lean against my ice packs and then as soon as they would get room temperature, I'd throw them in the freezer and then I'd lean on heat. And then I would go back and get my ice packs the next morning or, you know, at three o'clock at the end of the day after I did my visits. And I was just in so much pain and discomfort. I can't even tell you how much, but, um, They did. They found a tumor. It was eight centimeters by six centimeters by six centimeters, and it had started growing, they thought, in T11, and it had spread into T12 and T10. And so as that tumor grew bigger and bigger, it took my spinal cord's ability to have neurological pathways that were working between my brain and my legs and my bowel and my bladder. So that Monday... I was told I had a tumor. Um, and then by like Wednesday or Thursday, I was using a walker. And by Friday I was using a wheelchair because that tumor had grown that big, just insanity. It felt like, I, I did. Yeah. I didn't have any time to like, think
SPEAKER_02:about what was going on. Yeah.
SPEAKER_03:Oh. And I, I remember having a conversation with the doctor that day and like I said I was so uncomfortable I remember waiting in the waiting room I couldn't even sit next to my mom in the waiting room I had to pace the waiting room because I couldn't sit anymore like my pain was that uncomfortable that I couldn't sit anymore and it just it really did my tumor very much felt like an alien that had overtaken my body like it really did like
SPEAKER_01:For sure. Well, of course, because it's so outside the possibility of what you're thinking this could be, right? Yeah. Yeah. So did they do anything to help you with pain management between when they discovered the tumor and when you had surgery?
SPEAKER_03:Yeah. I was given hydrocodone.
SPEAKER_01:Hydrocodone?
SPEAKER_03:Yes. And I can't remember how many milligrams I was on. I don't think it was very many. Okay. And I think that too is another reason why Dr. Paul called for another scan because, oh my gosh, Heidi, that was not doing enough for me. It really wasn't. I remember I was taking ibuprofen around the clock with Tylenol because I think you can take them together at different times. Yeah, you can alternate every four hours. Yeah, one's an NSAID and the other is an amphetamine or whatever, or acetaminophen. So I... Yeah. My pain was not well managed when I got to Mayo Clinic. So that day I got my results. I worked a half day in the morning. I got my results at like one or two in the afternoon. And this is the Monday. This is the Monday. Yes. That I got my results that my mom was with me. She was driving me back to my apartment and she's like, yeah, honey, I think you need to call your work. And I'm like, yeah, you're right. I do. Like, I can't keep working and like fight this. Like I have a spinal tumor and now I can't walk. I kind of have to go. You kind of need to focus on yourself. Literally Heidi, I'm still up to this point thinking like, uh-huh. Yeah. But I can still work from the hospital. Like I was literally going to just take work home. And I had such an amazing hospice team. They were more than understanding. They let me take the walker and the wheelchair home and said, don't worry about it. We'll get it from you another time. you know, take your work laptop home to finish your notes that you did that this week. But like, don't worry about any of that. We will figure that out. Wait. So did you go
SPEAKER_01:back to your house or to your parents' house?
SPEAKER_03:So we went to my apartment, packed up three suitcases, and then I drove my car and my mom drove her car and we went right back down to Cannon Falls. At the time, my sister was living only an hour from Mayo Clinic. And, you know, when this happened, we really rallied together, my mom, sister, and, um, my, my, dad and my brother, we all rallied together and she was like, come move in here. Like, that's fine. You know, she was staying at home, I think a little bit more than, cause my nieces were young and my nephew was younger. And so it just worked out. And, um, you know, my sister kind of told me too, she was like, Tess, you don't need to go to the St. Cloud hospital up there. You know, it had like a three out of five stars, which is fine, but she's like, come down to Mayo clinic. Like you need
SPEAKER_01:a
SPEAKER_03:specialist. Yes. And so, That's actually one of the answers to the questions you had said was like, what would, what do you wish you knew ahead of time? And that would just be, you know, to all the people out there that might go through cancer down the road, Heidi, I'm sure you'd say the same, like find a specialist that you trust and that, you know, you might feel like, oh, this is, I'm really going above and beyond here right in the beginning, but like, we as women, especially when we're talking about like breast cancer awareness and cervical awareness, just as you age, having proper preventative healthcare assessment, like it's good to get checked out. And I would just say, again, these specialists have gone to years of schooling, whether that's an orthopedic surgeon or an oncologist that knows about your cancer. It can be the matter of life and death, right? Like what do you think about that as far as finding a specialist?
SPEAKER_01:I think, well, and I watched this, my sister was at MD Anderson in Houston and she had a specialist. He's actually at university. Well, he was at university of Iowa. Last time I checked, his name was Todd Janice and he was a special, a specialist in exactly what she had. He was a neuro-oncologist and she had a very rare tumor and, So her tumor was virtually 100% fatal. I think 80% do not survive the first year. And of the 20% who survived that first year, 80% of them are gone the second year. So it's almost 100% fatal, but she made it 18 months, which was amazing. And I think, I don't know. I just, my parents are like that. If we're going to do this, we're going to find a specialist. And so for me, I happened to be at a great community hospital. It's not really a community hospital. It's bigger than that. But a hospital that had a great cardiology program because my tumor was in my heart. And my cardiothoracic surgeon was amazing, Harvard trained, just amazing. He's fabulous. And then I love my cardiologist. They were great. And they and my regular oncologist from the cancer I had had before all said, you want to go to Moffitt Cancer Center in Tampa. It's a top 10 cancer center. And they have actually a soft tissue sarcoma unit. Wow. So they had, I mean, that was, I think of that as just a huge blessing. God put us here right when I needed to be here to have those particular doctors taking care of me. And what I had is 95% fatal. Yeah. So I had this 5% window, 5% chance, this tiny little window. And so we did whatever we could to get me in that window. And that's why we had aggressive treatment. And that's why I got so much radiation directly to my heart.
SPEAKER_03:Yeah. That's so hard. Yeah, that radiation and stuff. So tell me again, for the listeners that don't know your story, Heidi, talk about the three different types of cancer you had because you had a routine colonoscopy, right? And they
SPEAKER_01:found a tumor. So I had had a history of ulcerative colitis for years. But then I got out of a very, let's just say, very difficult marriage. And then I never had problems except around when I'd have kids. Because when you have hormonal changes, it can kick off those autoimmune things. And I'd been asymptomatic for eight years, but they still told me every other year. First, it was every year. Then it was every other year. Go get checked. Go get a colonoscopy. And so I did. And this was in Atlanta. And I had this great gastroenterologist who was like, yeah, well, you're coming up on your two years. And so I went and got it. And I remember waking up from the colonoscopy and him just, Dr. Friedman's sitting at the edge of my bed, just kind of like this.
SPEAKER_03:Yeah. I remember you talking about this in your first episode.
SPEAKER_01:Yeah. And he was just shocked. I mean, he said, people who present like you, we don't usually see a tumor. So for that cancer, it was adenocarcinoma. They took out, we had my whole colon taken out. They kind of rebuilt me another one. I had an ostomy, an ileostomy for three months. So I had a bag, which was my very least favorite part of this whole thing. And then they wait for the tissue to heal and then they go back in. They build everything and reconnect it, but they leave the, you have a stoma so that that tissue can heal. So all of my stomach contents was going into this bag basically. Yeah. Are
SPEAKER_03:you still using the colostomy bag? They were able to put everything back.
SPEAKER_01:And mine was an ileostomy, so it was slightly higher. Yeah. And I think it avoids some of the issues of a colostomy, but it was still, I mean, you still have green goop coming out into a bag on your side and you're trying to get it to stick to your side. And I was allergic to some of the adhesive and it was just... It was a nightmare. I know. For me, that was a nightmare.
SPEAKER_03:Isn't it wild how, yes, big of a deal just the skin is with bandages. It's like, that's never something you think about when you grow up using band-aid brand band-aids. Like they never caused a problem. Why? No,
SPEAKER_01:but some of the stuff in the hospital, I mean, it literally like pulls the skin off.
SPEAKER_03:Yes. Yes. I have scars from the sticker that went around my chemo port and stuff that I'm just like, dang, it looks like someone came at me with a fork.
SPEAKER_01:Yeah. Do you still have your port?
SPEAKER_03:I don't have my port anymore, but I have a scar here. I see yours.
SPEAKER_01:Yep. I see yours.
SPEAKER_03:Yeah. Yeah. Do you still have your port?
SPEAKER_01:Nope. They took it out. I had them take it out. I still have the, also the scars in the neck from the tubes when they did the open heart surgery.
SPEAKER_03:Yeah. How weird was that when they pulled out that port tube? That was bananas. That felt like they pulled a snake out of my arm.
SPEAKER_01:They did your port tube awake?
SPEAKER_03:Yeah.
SPEAKER_01:Oh no, sister. I was knocked out for that one.
SPEAKER_03:Well, that's good. Cause that is a really yucky feeling.
SPEAKER_01:Now I did have my chest tubes pulled after open heart surgery where they're like, and it's like, and that she's like, it's going to feel really weird and probably very uncomfortable. It's just like,
SPEAKER_03:Oh my gosh. Okay. So then after your Ulcerative colitis cancer because it was first ulcerative colitis and then it
SPEAKER_01:was. But I had had no symptoms and been totally clear on all my colonoscopies for eight years. No problem. Anyway, and so then I have this colon cancer. I have three major abdominal surgeries in a year. So they do the take everything out, rebuild it. Three months later, they do imaging to make sure all of it's healed in this new little fake colon they've made. I call it my Franken colon.
SPEAKER_03:I remember you saying that.
SPEAKER_01:So that's healed. So then they put my insides back on my insides because my insides have been on my outside with the stoma. And then later that year, 53 weeks from the first surgery, I had a preventative hysterectomy. Because I have something called Lynch syndrome, which is a genetic abnormality. And it predisposes you to colon cancer, uterine, endometrium, and ovarian cancers, epithelial cancers, et cetera. So that was the next one was ovarian. And the screening for ovarian cancer is crap in general.
SPEAKER_03:Did you know you had Lynch syndrome before? No,
SPEAKER_01:they found it in my tumor. They said there's this microsatellite instability in your tumor. And we want to check it because it can just be idiopathic, like random. Or it can be Lynch and I have Lynch. So
SPEAKER_03:yeah.
SPEAKER_01:Five years later, I was just tired. Like I was really kept telling Kev, I'm just so stinking tired all the time, but I figure I'm a working parent. I have a relatively demanding job. You know, I volunteered at my church, whatever. I was doing a lot of things. So that's why. So I went to, I went to BYU in Provo because our son was there. He was graduating and, And I went for graduation and I had this moment. Oh, and I also get bad migraines. We got T-boned in a car accident. So ever since then, I've gotten bad migraines. And sometimes it messes up your speech. And I hadn't had that happen for years, but I go there and for like 10, 15 seconds, I can think of words just fine, but I have articulation issues. And I'm like, huh? And so my mom and I were getting ready. The whole family didn't go to graduation, just me. And because long story, but you know, his, his dad and his stepmom were going to be there. We had young kids who were in school. It was, it just, it worked out better that way. So I'm there with my mom in the hotel. And I said, huh? I said, this just happened. She goes, oh, it could have been a TIA. Cause she'd had a couple. I said, well, it can also be a bad migraine. And she goes, well, call your neurologist. Cause I had a neurologist and he said, you know, just if it happens again, go to the ER. I'm like, sure. Fine. I'm going to graduation. So I went to graduation. And then I went on to Oregon for work for a week because that's where the headquarters of our company is. And I remember flying back. And I didn't think about this until well later. I flew the red-eye home and we stopped in San Francisco. And I remember just kind of feeling like my leg was asleep. And maybe it was, but I just felt like I was walking weird, like my leg was asleep. And then, okay, fine. But I just thought, you know, I'd slept weird. It was the red-eye. You're sitting on a plane trying to sleep. It's obnoxious. So then I get home on a Friday and the following Wednesday, I'm going to pick up lunch for me and our daughter. And all of a sudden I can't lift my right arm. And so I was like, what the heck? And, and I'd had weird, weird problems after the T-bone accident because it screwed up stuff in my neck. So I'd had, you know, nerve and other issues, but then I pick up my arm and put the pen in my hand. And when I write, it's just like up and down. like jagged lines. God crap. So I called Kevin said, can you take me to the ER? Cause this is what happened. He comes home from work. We go to the ER. And my brother, as I mentioned, is an ER physician and said, don't leave until they've done these five tests. So this is a satellite ER. The main hospital is about 40 minutes, 45 minutes away. And they did all but two. They didn't do the echo and they didn't do the MRI, but the CT was fine. My cognitive ability was fine. You know, like my neurology consult, they went through all the tests. I was fine. And so I had to make the choice whether to go home and go back at the next day or not. And I didn't, I was worried about insurance basically. I know sometimes when you check yourself out and then go check back in, like you're, you're kind, they call it like AMA against medical advice and sometimes your insurance won't cover it. So I'm like, great. So I had them transport me to the hospital. As I've said, most expensive Uber ever was like 800 bucks in the ambulance. Oh my gosh. We get there and they do the MRI. The MRI is fine. And they're like, well, we'll do an echo in the morning. So they keep me overnight in the hospital. And the next morning I go in and they do the echo and the girl, Alicia, she's done like three of mine at Sarasota Memorial Hospital in Sarasota, Florida. And she's great. So we're just talking, she's doing it. And she's a little, she's not, she's not giving anything away, but she's just a little subdued. And I get back to my room. My cardiologist comes in and goes, um, So you have a major tumor in your atrium and it was so big that on the echo, you couldn't even tell there was a tumor. It almost looked like an artifact, like the weird shadowing you'll get sometimes on ultrasound. And then when it turned on the flow though, you'd see this little tiny line of blood trying to go through. You know, when you look at somebody's ultrasound for a baby, you see the blood flow. Yeah. You, mine, you'd see this little tiny line going through and then it would spew out like a volcano. And it was like orange and yellow and purple and green colors. I'd never seen, I guess, because of the pressure or the speed at which it was coming out. And so they said, okay, so we'd like to do emergency open heart surgery on you tomorrow. And, and, and, You need to stay in bed, and if you get up for anything, have a nurse come. If you need to go to the bathroom, whatever, but we want you to move as little as possible. They think what had happened is little pieces of the tumor had been flaking off, and that's what had caused the stroke-like symptoms. Whoa. Yeah. The next day, they first had me go to the cath lab where they go through and basically— Check all the, it's like a plumber checking the lines. They check all your veins. Everything was fine. I just had this. They said, you're incredibly healthy. You just have a massive tumor in your atrium. And so they did the cath lab first. That's where I fell asleep. And I woke up. The first time I remember waking up is when they were moving me out of the recovery unit for open heart surgery into the cardiac critical care unit, CCCU or whatever they call it. Cause a friend of ours was a nurse there. And I remember Jerem being there and then I was out again. And so, yeah. And initially they had thought it was a benign growth called a myxoma. And then they took it to pathology. And I remember he came in and I'm like, it's more like, isn't it? He's like, yes. And I was just like, suck. Well, and you know, your, your sternum is, well, you know, with bone surgery, it's all fluid. I mean, they've stapled and wired your sternum together, but every time you move, I mean, it's, they give you a pillow to hold over your chest every time you have to move just because it's really, it's not pleasant.
SPEAKER_03:No. Well, and it's like you're probably still reeling from the first time you had cancer. Like that was still something you undoubtedly were still working through. And then to just be told like, oh, yeah, by the way, we're going to crack you open tomorrow morning after your breakfast. Like what? Oh,
SPEAKER_01:I didn't even get
SPEAKER_03:right. They don't even want to eat a vomit.
SPEAKER_01:But right. It's just and it was one. I mean, so the first time I had cancer, our kids were. 9, 11, 15, and 19. So this is five years later. So they're 14, 16, 21, and 25. Is that right? Yeah, because Chris will be 20. And so, and my poor husband, I mean, this is a second marriage for both of us. We've been married this year's 20 years. That's amazing. And he's, yeah, he is freaking amazing. I thank God for him literally every day because he is just amazing. the best thing in my life. And, and our poor kids have been, you know, it's like they came up to the hospital, you know, and basically we, you know, said a prayer and talked and they went home knowing I was going in for surgery the next day. And
SPEAKER_03:you might not. Yeah. Like, did you say you're good? You didn't say your goodbyes. Did you like, what did that look like?
SPEAKER_01:Not at that point. I just, I'll start to cry. I just told him, it's like, I want you to know that no matter what I love you. Yeah. Absolutely. Love you. A hundred percent. I don't think. And I had just this, I had this piece about it that didn't make a whole lot of sense, but I am a person of faith and I believe God can give us peace in the midst of really crazy, awful stuff. And I had the underlying, this is going to be okay. Eventually. But man, it's going to kind of suck
SPEAKER_03:for the next while. No kidding. Right. Well, I, I agree with you in the turmoil and in the uncertainty. I too felt like a piece that I can't even put into words. And I made the decision about my surgery because of the piece God put on my heart and mind. And I can't.
SPEAKER_01:So what decision did you have
SPEAKER_03:to make? They just said, they said in order for us to get that tumor out, we need to be able to get clear margins. And so we want to cut above and below the tumor, which would mean we're literally removing three vertebraes from your spine. And then we're going to put your leg bone in, your lower left leg bone in, broken in half as a new bony fusion, along with four rods and a bunch of screws. And so... Right.
SPEAKER_01:And did you know
SPEAKER_03:that
SPEAKER_01:would mean paralysis or did you know...
SPEAKER_03:Yes.
SPEAKER_01:Yeah. Yeah. They said you will be paralyzed if you want to go through with this.
SPEAKER_03:Yeah. And so we did my surgery. I was diagnosed like that day. I had my scan was like April 28th. Um, that's my birthday. Oh, really? Sorry. Yeah. That's, that's crazy. That's a crazy like parallel, but yeah, April 28th, 2014 is, I'm pretty sure if I look back, that was the Monday. That's the day I quit my job. And then, um, Like I said, I was at Mayo by that Wednesday. It was like May 3rd or something. And I got sidetracked. But yeah, it's just nuts.
SPEAKER_01:Because you have to make those decisions. You're getting hit with so much. And it's almost like the eye of the hurricane. Like you've got to find that place to be able to center yourself, so to speak. But just... be calm enough to make the decision. And all this stuff is just swirling around you in the
SPEAKER_03:meantime. Yeah, no, totally. It's like all of a sudden you don't care what was due, you know, three Fridays from that day, all of a sudden it's just like, okay, what are we doing? What does the doctor think we should do? Let me have a second to pray about this. What do I feel like I need to do? And anytime I was quiet because there were, you know, experimental surgeries, like we could have done, you know, a relieving of the spinal cord where they would like go in and remove tissue that wasn't my spinal cord in hopes that it could move freely again. And Pat, you know, I would regain some ability, but my tumor, we, when we biopsied it, it was malignant as well. Super low chances for survival, super high with sarcoma. Yep. Super high for lung or going to your heart or wherever. Right. Right. And so, um, Yeah, I just like you, Heidi, I just had this crazy piece about the decision to what are the best odds at survival? And it was the surgery. Yeah, you have to be in a wheelchair the rest of your life, but you might beat cancer. And so I chose to do that. And it sounds like you chose to do that, too. You said, yes, take me to surgery in the morning. So did they get clear margins? What now? Talk about the third cancer, too.
SPEAKER_01:Okay, well, they didn't get clear margins. It was close. I mean, he said, I took my cardiothoracic surgery. He said, I took everything out I possibly could and still repair it. He said, it's the biggest bovine patch I've ever put on a heart in 25 years. So they take cow tissue and they patch the place he took out. So it was almost clear margins, but there was one place where it wasn't. And so then I went to Moffitt and And I met with Dr. Brohl. Andrew Brohl is my sarcoma specialist. And Arash Nagavi is my radiation oncologist. And so the recommendation was radiation for... Well, the first one, and they said it's basically almost 100% fatal. And I'm like, then why would I do chemo or radiation? That makes no sense. And he said, no, you have... I'd spoken with some other people ahead of time. And then he goes, Dr. Brokham. And he goes, no, there's just five. There's just a little chance. I said, like what? He goes like 5%. And he said, you have to be really aggressive. But if you happen to get in that window, the, the outcomes, if you can, if you can do this and it works, he said, then the outcomes could be really good, but it's, it's a slight chance, but if you want to take it, that's the shot you have to take. And so I, We did 60 gray. So we did two gray. It's a, it's a measurement of radiation, but two gray a day directly to my heart. And then I did three rounds of chemo with gemcitabine and docetaxel. And they're both very, they're, they're particularly strong. Yeah. Chemos. Did you do chemo? Yeah. Oh, yeah, you did. I remember because you're talking about
SPEAKER_03:your head. Yeah, no. And I know it's really... It was kind of weird because I was diagnosed and... April, kind of came up with a plan in May. And then the surgery was going to be like June or July. And then we didn't have the team we needed. And we thought maybe another round of chemo might be good. So my doctors kept making my surgical team and we waited one more month. And so I did have a lot of chemo and
SPEAKER_01:pre-surgical surgery.
SPEAKER_03:Yeah, presurgical. And so they wanted to see if the chemo would shrink my tumor a little bit. And it made the outside kind of necrotic or dead, but the inside was still very active, like on my pet's hands, which isn't surprising because after my surgery, they showed me images of of my spine and like it I'll have to send you I will send you Heidi the images and I'll put them on my website too but they I mean so they had they had it sliced you know
SPEAKER_01:plane by plane by plane
SPEAKER_03:yeah by plane by plane so parallel with the ground if you were standing up and so these big round you know cutouts of my spine and it's like a vertebrae should be like the same size as like a tennis ball. Like it would fit into a tennis ball and it had grown so much wider than that. You couldn't even make out the wings on my bones. Like the tumor was just completely over the top of that. And so I'm so thankful that they got clear margins. Cause I don't know, you know, and it's crazy when you look at your MRI and they're going down plane by plane again through the machine like okay here we are it's like holy cow look at how close my kidneys are look at how close my stomach is look at how close my lungs are I mean jeepers this was like right below my heart like back there it's just how did that not spread Heidi I don't know but I really like I said so was it kind of encapsulated Yeah, kind of. They knew it had grown from my spine or started in my spine. It was coming from there, but it was just very odd the way it grew. It was elongated over those three vertebrae. It looked like it had grown out of the one and stretched to the other.
SPEAKER_01:But this way rather than...
SPEAKER_03:Yeah, rather than round. It was oblong.
SPEAKER_01:Mine was too, and it was kind of encapsulated. They said, this isn't a typical-looking sarcoma. Yeah. It almost had like this sheath over it. It was really weird. I'll see if I can find pictures.
SPEAKER_03:Yeah, it'd be interesting to see. Okay, so they didn't get it all out of you though, but they were able to do the radiations and the chemotherapy. And
SPEAKER_01:there was nothing visibly there, but it was just a pathology they found.
SPEAKER_03:Right. So like, what does that look like today, now?
SPEAKER_01:Well, I have, I mean, I still get... pet scans every three months because I have weird stuff that happens in my heart. Still. I have a, um, call it a sanguine assist. My friend, Angela calls it a zit, the heart zit, but it's basically like the bovine tissue, the cow tissue didn't like radiation. So it formed
SPEAKER_02:this thing
SPEAKER_01:that they first thought it was a tumor recurrence, but it turns out it's
SPEAKER_03:not. And
SPEAKER_01:yes, I do. Right. I know you
SPEAKER_03:do. I know.
SPEAKER_01:I have another spot that's weird that they're watching too, that has gotten slightly less metabolically active and slightly smaller. And so we just do a lot of screening and then, um, and soon after the surgery too, I had to have a bronchoscopy where they go in and take out some tissue from your lung because there was a spot that was weird there. So they think it's, we're hoping it's just inflammatory stuff, but we just have to watch. And, and I, I was praying about this at one point and I got the impression, just you're not going to have certainty. And I don't like that. I hate that at all. It is. It's hard.
SPEAKER_03:We all want control.
SPEAKER_01:Oh, for sure. But I got that. You're not going to have certainty. So you need to learn to live in this kind of limbo and still be happy. Yeah. And so far so good, you know, not what is it? Wallboard.
SPEAKER_03:I've got wood.
SPEAKER_01:Yes. Thank you. So far. I mean, I feel like I've been really blessed. It's not easy. But anyway, and then they found in one of my PET scans, they found the urothelial cancer, which is basically your ureter connects your bladder and your kidney, as you know. But for those who don't know, that's what that does. And mine is right at the base of the kidney where the ureter starts. There was this mass and they found it because of a PET scan. And it doesn't really show up well on a PET because you excrete all that radioactive glucose out. through your kidneys and your bladder anyway. But there was just something that was off when the radiologist saw it. And so they had me do a CT urogram, which checks specifically for that. And I did have a mask there. And the doctor said, due to the size and shape and placement, you're probably not going to be able to get it by just going up through your bladder. We're probably going to have to do another open abdominal surgery, which I hate because I get adhesions and it causes bowel
SPEAKER_03:obstruction. Oh, it's so traumatic to your body.
SPEAKER_01:It's really hard, but... Um, he got in there, he said, I'm going to have the laser there just in case. And he got in there. And when I got out, Kev said, babe, they got it. They were able to get it. So, and, and I just had another surgical check and it was totally clean again. So that's been almost a year of clean and clear and looking good. Yeah. So it's just like, it's, it just becomes stuff on your list, right? You know, you go for scans every so often. Do you still have to go and do pets? And
SPEAKER_03:yeah, now I'm just doing, um, Well, I was doing once every six months. Um, this is the first time Heidi, I was checked in July or June and I will wait until June or July of this year. Wow. Yeah.
SPEAKER_01:That's something to celebrate because that means everything looks really good.
SPEAKER_03:Yeah. And I've been really proud of myself to not worrying. Cause I know I'm sure there have been times where you're like, it's not time yet, but I'm worrying because, you know, it's like, I don't know if you're like me but it's like every little twinge that's different now you're like
SPEAKER_01:dude when you're talking about your lower back hurt I'm like my lower back's been hurting it's like I've also been sitting in a chair for eight hours that'll
SPEAKER_03:do it that'll do it
SPEAKER_01:but but it's just I think once you have it happen you're You have to fight that hypervigilant because you can't live your life worrying about every twinge. But there are moments where that happens. That's actually one of my next podcasts is going to be with our therapist about anxiety. Anxiety in general and then anxiety around... Moments of crisis and how you manage that.
SPEAKER_03:Yeah. Well, and I was going to ask you, like, have you had and then we can start going through your questions, too. But I was going to ask you, have you had moments of trauma? I mean, obviously losing your sister when you guys were in your 20s must have been horrible. Yep. Did any other moments? thing in your life help prepare you for the trauma that you describe as like the eye of the storm and having to really just focus on the here and now like I know being a parent I'm sure has given you a unique perspective at life but
SPEAKER_01:my first marriage was let's just say very very unhappy and I had to not only be that eye of the storm for myself but be that for my children yeah And that's, I mean, that's something that did it. Going through cancer with family members and friends, that did it. Just, I think, I don't think everything necessarily happens for a reason. Some things just happen, but I think you can find reason and purpose there. and wisdom in anything. Does that make sense? Yes,
SPEAKER_03:it does. I would agree with you. Yeah, some things are horrible and never should have happened. And we would never say that that happened because, oh, now look, you can give$5 to this homeless person. Yeah, that's not what we mean. We just mean that these horrible experiences allow you to put on a pair of glasses that just helps you see things differently. And yeah, it's horrible, but it's also really amazing that like, in some ways we can understand people going through hurt that another person couldn't because they just haven't been there.
SPEAKER_01:Right. And not be, not that they wouldn't if they went through it, but it's just, I think that's also why it's important to share your story. Cause I think people, um, sometimes worry that it's a sign of weakness or whatever else. It's like, yeah, it kind of is. I'm probably a lot weaker than a lot of people. So what?
SPEAKER_03:Yeah. Well, I think you're stronger. I think you're stronger for it. I think there is advice and wisdom that you could give someone that they might need in a week time. Like, yes, we are, our bodies are humanly not going to last, right? We, especially as people of faith believe that, but it's pretty amazing that you can step in and be a rock for someone else when they need it, even though. Well, you too. I can't,
SPEAKER_01:I have to tell you, Tess, I can't imagine. I can't imagine my mobility changing overnight. Like I, I, I can't even wrap my head around that. I have friends we knew when I was a kid, two different friends, who in accidents, one was a car accident, one was, I believe it was lightning that hit a tree and fell on her as a child and she was paralyzed. Oh my gosh. And in both of those, it was so quick and so fast. And I've seen the grace with which those people have built their life. you know, they've just, they've built a life and they have issues that they have to deal with as a result. And, you know, maybe there are sores or this, because it's a certain place that's rubbing or whatever, but they've built these amazing lives. And then I think about you having to choose that. Yeah. And, and I just, how did you, I mean, did it feel like an easy decision for you or did it feel like something you really struggled and agonized over?
SPEAKER_03:It felt like an easy decision because of the faith God put on my heart and the peace he put in my mind. I mean, I remember my doctors and my whole family sitting around me in a room about the size behind me, you know, a living room size. And there was six doctors in white coats and then, you know, a family of five. We were kind of one half moon and they were the other. And I remember them, you know, all saying like, are you, What do you feel? What is your decision? And I'm like, I want to do the surgery. I want the best chance at survival. If I choose one of these other options, there's a larger chance you're not going to get the whole tumor out. So let's do it. I mean, I trust you guys. I trust your advice. I want to get better and I want to fight it. And I know... Right. I know... Not everybody gets so lucky, Heidi. There are people that have had both of our surgeries that haven't made it out of the operating room. And so, you know, it's hard for me to know why, and I don't know why only God does, but I, I 100% would have struggled with that decision if I didn't. If you hadn't felt that. Yeah.
SPEAKER_01:Yeah. Yeah. And I think that's, I don't know. The big decisions, not that they were easy, but they were clear. I think that's what I'm trying to say. Yeah,
SPEAKER_03:like you knew you had to have the heart surgery. They couldn't just ignore that.
SPEAKER_01:For real. Yeah. Yeah.
SPEAKER_03:And maybe
SPEAKER_01:it was like, kind of like, well, this sucks, but I guess this is what we're doing tomorrow. And
SPEAKER_03:I mean, yeah, there, I definitely felt that. I mean, I had, I remember the night before I went in for my surgery, we got a hotel room at the Mayo campus and we thought like, okay, well, this will be good. Cause then we'll just wake up at four or 5. And go walk across the skyway to the hospital. We don't have to drive. And it was, that was amazing. the most unsettling time was when I was putting my gown on before going back. I remember I had a little bit of doubt and a little bit of fear then, but I, I knew it had to be done. So did
SPEAKER_01:you, did you do anything different or special or whatever the night before, or were you still just in so much pain that you just were not able to do much of anything? Um,
SPEAKER_03:My dad and I had talked about going to the hot tub, and I think, honestly, the day was just so exhausting. We ordered, like, pizza, and I think I might have made a couple thank-you cards, and we kind of laid down. Of
SPEAKER_01:course you did, because the night before you have a massive surgery, you need to make sure to get those thank-you notes out. Right? Your mother would be so proud. I know.
SPEAKER_03:Oh, it's just, like, ridiculous, but... Yeah, I think it was really hard for me, too, to just wait. You know, I chose the surgery and then I had to wait like three or four months. And I did. I got worried, too. Oh, I couldn't. I don't know that I could. I got worried that like that tumor was going to spread. It was going to, you know, do something else like. Right. So. I don't know. It is. It's just it's so hard. I and again, my social work background is. my love for gerontology and older adults and the study of equality and diverse groups, I just really felt like this podcast would be something that I could do that was feasible, that would help me make connections with other people. Because over the last seven years since I was diagnosed, I feel like I've been so inspired and so uplifted to find passion in my own daily life when I hear stories of other people overcoming and being resilient with whatever it is you know I couldn't be I couldn't imagine being a parent and like seeing your kid die of cancer or you know I couldn't imagine losing a baby within the first three months of life to SIDS or you know there are all these things that happen and we don't know why they happen right but If we can just find some type... Sorry, just a second. No, you're fine. We have dogs. Midge, come here. What was
SPEAKER_01:I saying? You were just saying there are so many things that other people have been through that you can't imagine.
SPEAKER_03:Yeah, they're horrible things, but it's just like... I... I'm... I'm so happy to hear people's stories of overcoming around it. I don't even really know what else to say about that, but I just felt like I did. Heidi, I think too, I'm like, gosh, if the pandemic would have broke in the fall or the fall before I started, I may never have started my podcast. When we talk about God's timing, it must have been so hard for you too to get everything up and going during a pandemic, but maybe that was the push that you needed to start.
SPEAKER_01:I don't, I, I had, I always tell people mine are highly underproduced because it's like, I don't, I don't know what I'm doing. And I had friends, like I, I was telling you the people at work, the guy at work, it was like, Oh, you might want to look at this microphone. And the guy at work who was like, Hey, you ought to look at this squad cast to do for your thing. And people were just very kind. And I just said, look, I'm just doing this in my walk-in closet people, but I, I'm hoping that the quality of the story outweighs the quality of the
SPEAKER_03:audio. Well, it will for mine since I just had my dog barking on here. But I love what you said in your first episode, too. You're like, you guys might hear my family. You might hear my dogs. But you're going to get genuine. You're going to get vulnerable. That's what you get with me, too. Well,
SPEAKER_01:because I think especially when you've gone through things that are life-changing at a very... visceral, basic level, it's like, I don't have time for fake. I don't, I try to be nice to everybody, but I really have a hard time with people who are false.
SPEAKER_03:Yeah, I know. And it's sad, but it's like, it's only a matter of time before life. I mean, how do you, how do you be emotionless and disingenuine and fake when you're Life throws so many challenges. Like, I literally wouldn't know how to be fake if, you know, like, there's no way you and I could have done, could have fought the fight we fought with fake. No, and fake our way through. Right. It just doesn't happen. What do you wish you knew ahead of time? Like we said, go to a specialist. For me, it was listening to my body and trusting my body and advocating for myself. You know, that doctor was like, go to PT and you're But your abdomen isn't strong enough. And for me, it was like, are you kidding? Like, I'm running around. I just got out of doing high kick dance. And, you know, sure, I had fun in college, but I don't think all my abdominal muscles went away in college.
SPEAKER_01:Suddenly disappeared. Right. And I think advocating for yourself in that way, because I think especially, well, and I think it's particularly an issue in the U.S. where we don't have... universal health care. And so, you know, there's a cost involved and you're new in your career and you're trying to be prudent about how you're spending your money. I think I hate sometimes that those factors come into our heads before we think about, no, I really ought to go get this
SPEAKER_03:check. Right, right. And obviously your life or my life is worth as much as an MRI scan. So anyone else's that needs it, I agree. It's like, we could talk all about healthcare in this country. And I agree, there are so many things we could do differently. And isn't it sad that, you know, a local shelter is kinder to the animals than we are to our neighbors, as far as healthcare is concerned, like, you're spot on about that. And so, you know, one thing I wish I would have done differently, or, or known ahead of time would just be, yeah, gosh, I should have trusted my body and pushed for that MRI quicker. And if that doctor wouldn't have given it to me, I do. There are days I wonder, Heidi, and I know what's happened in my life has happened for some reason. I'm not saying everything happens for a reason, but for some reason, I went through what I did. You know, we can't obsess too much over our past because It would ruin you. You get that with the first marriage you had. If you focused on the negativity and the toxicity that was that marriage, you wouldn't be the survivor
SPEAKER_01:you are today.
SPEAKER_03:And I
SPEAKER_01:wouldn't have gotten to be this person without going through that. And that taught me lots of things. And honestly, I've told my kids, even knowing how it was going to turn out, if it took that to get me to this, I would go through it. I'd be irritated probably a lot.
UNKNOWN:Right.
SPEAKER_01:But I'm very happy and at peace with where I am right now. And that's a huge gift.
SPEAKER_03:Yeah, it really is. You can't, there's no price tag on experience. I fully 100% believe they're just, yeah, there's no price tag on that. And the thing that kind of goes along with and our journey and our experiences. The other note I made under that question was, I wish I would have made a timeline journal of my story, how I was feeling and what I was experiencing. It matters so much. And after all the trauma you go through, sometimes you forget the order in which something happened. And I don't know about you, did you keep a journal during any of your cancer experiences? Fights or not really?
SPEAKER_01:Yeah, some of it. When I'm right in the thick of it, though, it's kind of all I can do to just get through and do the stuff that has to be done. And I kept working. I mean, granted, I was only working halftime and I was answering questions. Once I was conscious, I was answering questions on my phone. People at work and they're people like, stop it. Don't do that. I remember in with the first cancer surgery, I was in recovery for like eight hours because they didn't have a bed on the floor. So I was in recovery. It was just me and a couple of the nurses. And I was texting people back and my boss at the time goes, Heidi, just like Heidi, put your phone away. You just had surgery. I'm like, yeah, but I'm doped up. And I, and my emails.
SPEAKER_02:So let me respond
SPEAKER_01:to that. And so I just think it's, I wish I had done more about it because I'll tell you, for me, one of the worst things is I was taking benzodiazepines and I had no idea how addictive they were. Yeah. So it's just like Ativan for nausea and a little bit for anxiety along with some other things. And I happen to have a hospitalization. Me too.
SPEAKER_03:They put me on Oxy right away when I got to Mayo. You know, I was like, man, doc, this Tylenol, Ibuprofen and Hydrocodone are not doing it for me. And they gave me Ativan and they gave me Oxy. And it is, you're right, that stuff is nasty. Like it does what it needs to, but it
SPEAKER_01:is,
SPEAKER_03:it's nasty stuff.
SPEAKER_01:I don't know that I do benzos again, you know, Ativan, Klonopin. Xanax. I don't know that I do those again, unless it was like a one-shot deal just for a thing, but I had, I was on it for a while. Around the clock,
SPEAKER_03:you were on a schedule of it
SPEAKER_01:or? Well, I kind of, and I, and I alternated it with, um, I can't even think of nausea. You know what I mean? The main thing for nausea. Oh yeah.
SPEAKER_03:They gave me like Zofran or something.
SPEAKER_01:Yeah. So like Zofran, Ativan, and there was one other thing and I would cycle through those during chemo. and part of radiation. But then I had to go in the hospital and it was a hospital that my oncologist didn't have privileges that it was the one closer to me. And they didn't have that in my meds for some reason. So I was off of it for 10 days. And then I had this rebound anxiety that was horrific. And I had my oncologist and I worked on it. Yeah.
SPEAKER_03:That's awesome though, because you're right. There's a huge difference between just regular anxiety and anxiety brought on because you're going through a withdrawal. I mean, that is really uncomfortable. Yeah.
SPEAKER_01:it was horrible and it took months to get off. They had to put me on something else so I could taper off the benzos. Um, and I know a lot of people, I feel very grateful. I was able to get off of them because a lot of people just can't. And I understand that they can't sleep their bodies. So yeah, them to it. Yeah. But, um, but that, that and the ostomy and waiting for my, waiting for my chest, like my sternum to, fuse again. Those are probably the three worst things besides facing death and trying to figure out what you're going to do. And, you know, but as far as physically, those three were the worst. What about
SPEAKER_03:you? Physically, for sure. My incisions were the worst too. Yeah. You know, they literally cut me in half. took out all my organs, put them next to me while they're cutting me in half, you know, fixed my rods and plus the leg inside. Like they've fixed the rods inside my cavity to attach the ones from the back. Like, like just, yeah, the, the incisions took like seven months, I think to fully close. They were packing a back wound that like, you know, was huge. And then it was the size of a straw. They were packing that. And, um, for me to, again, just like going through such a big surgery when months before I could walk on my own two feet and then being in a wheelchair, it almost felt like if I would have just had a spinal cord cord injury, um, I feel like it would have been easier, but with the cancer too, it was
SPEAKER_01:just very weird. You're fighting on multiple fronts and it's not like, it's not like you just happened to lose mobility. It's like, you've got to heal from the inside out from this massive, massive surgery that not, I mean, and you've got multiple sites that have to heal and that's a lot.
SPEAKER_03:It was a lot. Well, gosh, Heidi, you too. I mean, going through three, Yeah. Three different
SPEAKER_01:cancer sites. That's. Yeah, but not at the same time. Yours was all at the same time, kiddo. Well. I say kiddo because I'm, you know, 20 years old.
SPEAKER_03:You're allowed to. I'll let anybody that has kids call me kiddo. I'm fine with that.
SPEAKER_01:I call anybody that's like my children's contemporaries or around that age kiddo. So I apologize. I don't.
SPEAKER_03:I'm not
SPEAKER_01:offended. But I mean, you had, you were, I think mine was done in a series. you were kind of doing that crammed into one. I mean, how long was your surgery? It had to be. Oh yeah.
SPEAKER_03:It was over three days. I had one, like one day in between as a break, but I think they were like, they were 12 hour surgeries on either side. So.
SPEAKER_01:And did you, were you conscious at all during that? I
SPEAKER_03:woke up for a little while and I was doped up out of my mind too. And I remember I was writing things down to ask questions about how my first surgery went because I I had a tube, too. I couldn't talk. My mom finally took my notebook away and was like, honey, you're going to just relax now. I can only imagine. You're wired. I'm already a wired human. I'm all ready. Me too. Super lit up from talking to you. And I am lit up from talking to my doctors. And I'm just like, oh, it went all well the first day. Great. Tell me this. Tell me that. And they're like, okay, you're not going to remember half of this. And you're like, I don't care, but just tell me. Right. We're right here. Exactly. I'm not going anywhere. But yeah, I would say... make a timeline journal. I know people are probably like, I don't want to make a journal during the darkest time of my life, but you never know how God will use your story. And, you know, for me, I realized one thing on my bucket list too. You had asked me, what items do you have on your bucket list? And I really wanted to, I really want to write a book before I kick the bucket entirely. And so I just think it would make it so much easier if I had a book. I mean, I,
SPEAKER_01:No. Yeah. I've talked about it. That's why I'm doing, I told my friend, she's. Well, you got to do it too. Well, but it's like, that's why I started the podcast is I'm like, I just don't have the mental space right now to do a book. Yeah. But this I can.
SPEAKER_03:It's like, yeah, we get energy from hearing other people's stories before we can really write our own, I guess. But yeah. So, okay. So that, that kind of wraps up. general info, tell me your story, things you wish you'd have known ahead of time. The last thing I have actually on that one is I put read books. You know, if someone gets diagnosed with a spinal tumor or, you know, a spinal cord injury, if someone goes through a spinal cord injury, there are so many people that have lived through debilitating health journeys. And so I would just say asking friends and family what they would recommend to you about that because it can be really hard to you know a lot of times people will say like I feel so bad I don't know what to do I don't know what to say but like just you being able to sit and read about someone else's experience can be really empowering and so
SPEAKER_01:and I think I don't know about you but I found a lot of people kind of came out of the woodwork yes that I didn't know had had cancer or had major trauma or had you know great losses in their life and they they were kind enough to be vulnerable and share their stories and it helped me feel like no no other people have gotten through this you can yes you can get yes
SPEAKER_03:absolutely absolutely yeah um like I said, my mom was a nurse for 30 years. My dad was a teacher for 30 years, um, all in the town I grew up in. So yes, people, you know, like my old Sunday school teacher, my old fourth grade school teacher, you know, I got cards from them and it just felt like, wow, like you care enough about my journey to like sit down and write some encouragement. Like that's pretty beautiful. And so I would agree. I, um, People gave so much money and sent my sister a gift card to the co-op so she could just go buy groceries that weekend and not have to worry about the money. It's hard accepting help from other people, but people want to help. And I would say for sure that is something that I would encourage people to openly accept and Yeah, even when it's hard. Yeah, and we all know, like, if our neighbor gets sick or, you know, the little old lady from church gets sick, you know, you would do the same thing. And so just being open to that, I think, is really good. You know, you would ask me too, Heidi, what have you learned so far about yourself, life, cancer, etc.? My... presence is valuable. My time matters. Energy is sacred and something that I need to respect and protect. And I
SPEAKER_01:need you to write that down and text that to me later because that's really profound. Well,
SPEAKER_03:I literally just wrote it like today under that question. And in fact, that's the only thing I have written for that question. Um, But I do, I feel really, and maybe that's because that's something we as people without trauma learn over a lifetime, how valuable time is. But I guess I just really feel convicted to share that. I mean. It
SPEAKER_01:reminds me. Okay. So when I was starting radiation, so we were driving 90 miles each way. Every day. And, um, our kids were at camp and this is about a month and a half after I'd had open heart surgery. So Kevin, I had some very real, very, I mean, we're very honest with each other anyway, but we had to have those conversations about, okay, what, what say you don't make it, or we find out this isn't working. You know, what do I want to do before I go? And, um, how do I want to spend that time? And so when you said that, you know, about how precious time is, it's like, you never feel it. So, and I know this is very cliche, but you never feel it. So viscerally until you think it's going to be. Yeah.
SPEAKER_03:Well, and you, the eye of the storm, you said it so perfectly. It's like stuff was going on in your life. And then all of a sudden you looked up and you're like, Whoa, what really matters right now? Like not, Not any of that stuff, not putting on makeup today and not doing laundry. Like,
SPEAKER_01:as you can tell, no, putting on makeup did not matter. I
SPEAKER_03:showered today and I put on mascara. So that's what you're getting from me. That's, that's all I came here with. But you know what? If, if that, if that little, because now here's the other thing that comes up with the disability piece is like, gosh, darn it, Heidi. I wish more people knew that if they had a working brain in their heads and Working legs and working hands, there isn't anything you couldn't do if you believed in yourself. And that feels dumb and cliche too, but it's true, dang it. Like, isn't it sad? It is. Yes, even just on a very, you know, basic thing that a lot of people can understand, bullying kids in school. Like, why are we doing that to one another? Why are we casting such hate on one another? Yeah. the very God-given abilities you have could do so much more good than bad if used in the right way. I remember feeling that really. I liked your word viscerally. Even just, again, the faith of the Mayo Clinic and of your hospital. I'm sure when you're there and when you're healing, I don't know if you had the same experience as me, but I just felt like this Holy sacred presence that like, no matter what, even if I died, it was going to be okay. And my family was going to be loved and I was going to be cared for. Yeah. And the time those nurses give, isn't it just incredible?
SPEAKER_01:Well, they're amazing. In fact, one of my favorite, favorite nurses at Moffitt, Lori, she actually did one of the podcasts. She's in radiation oncology and she was a pediatric hospice nurse for eight years. And that is something I just really admire about her because I think that is one of the hardest and most generous things you can do is help a family and a child through that transition. Oh,
SPEAKER_03:yeah. Again, some of what I do, and this is no slam on you, but some of what I do feels... silly, right? Because. Oh, no, that's not
SPEAKER_01:a slam. I feel like
SPEAKER_03:that. Yeah, it's like we're still alive. And so it's weird. It's like, gosh, Heidi, do we feel guilty for being alive? I mean, I don't want to say I feel guilty, but I think you and I just have a very realistic outlook that like not everybody gets a second, third, fourth chance. And so I wonder for you with the reoccurrence of reoccurrences of cancer, you've gone through, what gets harder and what is stronger about how you react to a situation because of what you've been through numerous times? Does that make sense?
SPEAKER_01:Well, I'm working on not freaking out as much when I get a diagnosis. And I look at it like maintenance. Kevin and I have had this conversation numerous times, my husband Kevin and I, These things are going to come up. Once you've had cancer, you're going to have weirdness. I mean, it just weird things come up in your body, whatever. The one thing I would say is I try harder not to freak out about it and view it as just like, it's like a tune up for a car. Like I said, you're going to take, I think I said this another one, you're going to take it into the shop. Sometimes things are going to be fine. And sometimes there's going to be something major that has to be fixed. And then it just kind of becomes a thing on your list. Yeah. Like, I mean, I think about like I lost, well, he's my nephew, everything but blood wise, but the son of dear friends. And she's like a sister. She's my sister. And Quinn fought neuroblastoma for seven years from when he was five to when he was almost 12. You know, I lost my friend Valadia to glioblastoma. My sister died very young. you know, and I lost dad, most of the people in my dad's family live into their hundreds. I'm not kidding. Like they're working in their mid nineties. So it was very shocking when dad died early. And I think there are a lot of things I have to deal with as a result of the surgeries and the cancers and whatever else, but I'm not dead. You know, I get to wake up in the morning and I get to love my family and hopefully help make the world a little bit brighter place for the people around me and a do a job at work that helps to make the, you know, our whole thing at work is protecting the world's water and do something that makes the earth a little bit cleaner. And maybe I can provide some good and I have that opportunity. So while the things really irritate me sometimes and my limitations irritate me, sometimes they aren't that big of a deal, you know, really in the big scheme of things, they're not that big of a deal.
SPEAKER_03:And then the harder parts, what are the hardest parts then? Physically, your scarring and stuff?
SPEAKER_01:Physically, my lungs are pretty scarred up. So I have to be very careful if I lay off. I take walks and I ride my bike and stuff and I swim in the summers. Good for you. Or tread water. Yeah, just to try and stay mobile. But if I lay off, you can feel that scar tissue just tighten right back up. Is
SPEAKER_03:that a sensation you feel in your back or mostly in the front?
SPEAKER_01:mostly in the front for me. Um, and also just, just lung capacity wise, you can tell when you're breathing, you're just really tight. I get
SPEAKER_03:that. I don't know the degree that you understand it, but with my paralysis, my like diaphragm doesn't stretch as much. And that can kind of be an, an, an anxiety and do you feel that way? Just do you feel some days like your mind is, not as good at coping because you're physically different.
SPEAKER_01:Yeah. Oh yeah. That happens. And you just get, it's, it's, you have to fight that discouragement. You have to think about what your body can do, not what it can do. And I mean, like I said, I admire you so much test because huge mobility issues. I don't know how I deal with it. I really don't. And I just admire that you've kind of like, okay, this is what we're doing. I figured it out.
SPEAKER_03:And thank you. I, you know, I have sometimes said this about my mother and I want to reiterate to your listeners that might go find my podcast or vice versa. Your listeners, my listeners will go listen to yours and whatever that, you know, I never want to make my mom feel bad or, um, you know, like she's crazy or something. Cause she's dealt with depression her whole life. And when I got sick, it's been really hard for her to, um, find joy in the overcoming and in the resilience that we've done as a family. And some days it, it's enough to make her really sad, but I never want her to feel like, I think she's crazy, you know? Um,
SPEAKER_01:No, but you think of the weight. Can you imagine the weight of going through that, watching your child go through it?
SPEAKER_03:But mentally, my mom is dealing with the depression. And some days that is more paralyzing than my physical limitations.
SPEAKER_01:Yeah. Well, did you feel like that when you were... For me, getting off benzos, the anxiety was... And I had had... I mean, I think I tended to be a little bit more anxious kid than maybe some kids. And I had had like a panic attack once when I was going through my divorce. No, twice. Well, see, that's scary. That... And those were kind of scary. Right. But it was different than getting off the benzos and having that rebound anxiety where it's all you could do to focus on inhaling. You're just trying to take the next breath. And it gave me so much admiration and compassion for people who are constantly dealing with that kind of anxiety, not necessarily due to circumstance or reason, pharmaceuticals like i was but that's just you know biochemically that's what they're dealing with and that's the reality yeah and i just
SPEAKER_03:isn't that insane i can't even yeah that that was such a light to you and i you know one of my i think it was my second no third third podcast episode i interviewed this pastor and he talked about how when we're rejected or when we reject some like say for their sexuality, sometimes that is more hurtful than all the love they've ever gotten. And it's like, Oh yeah, our brains are so fragile. They're so incredible. And so, um, you know, full of ways to adapt, but they're also,
SPEAKER_01:but just neuroplasticity doesn't mean the hurt doesn't hurt.
SPEAKER_03:Yeah. Hurt. Yeah. Yeah. And so, um, Yeah, just the comment about my mom. I hurt for her so much because now the further out I get from my surgery and the further into disability I get because now I've reached this weird plateau in my life, I feel like, where, okay, now I don't have to worry about cancer, but I still have to worry about my disability. So here I go. You know, and it's like, oh my gosh, like my hips are getting tighter. So I'm having more back pain again. And I feel that in my abs. And gosh, if I don't lift my butt up, like I should have lifted my butt up once already while talking to you. And I haven't done that, you know, pressure relief, like just the small things and maintenance that we can do better for ourselves. I'm sure for you drinking more water and making sure you're taking deep breaths and keeping your whistle wet. And, you know, it's
SPEAKER_01:just... That maintenance is like a full-time job, honestly, sometimes it feels like. It is a full-time
SPEAKER_03:job. This disability is a full-time job. And so now I need to find value in the things that are most important to me, prioritizing what's most important to me. It says favorite places to be. That was your last question. Being with friends, being with family. In parentheses, I put when we're getting along. In the sunshine, around the outdoors or a campfire, singing songs, being at home with my dogs, doing art, being around children in my family. You know, if time stood still tomorrow again and I was re-diagnosed, those are the things I would do immediately. It wouldn't be reaching for my computer anymore. As a 24 year old working in a job she loved. And I think it's beautiful that like one of the things that gives me passion is serving others. And I think you are the same way. I hear that about you. And again, you being a mom, that is obvious. And so now how do you and I keep living our lives while making sure we're touching these priorities and But how do we also pull the people we love along with us to do these things with us when they aren't there yet in their healing? Has that been hard for you? Like even the loss of your dad or your sister? I know that was so much so long ago, but that hurt is still very real. I'm sure for you. Oh,
SPEAKER_01:yeah. And doesn't it? For me, it feels like I don't quite know how to articulate this, but it feels like those wounds have definitely scarred over. But when I got diagnosed or got diagnosed again or again, it opens up that wound again because it, and, um, because I think, I think I said this in a podcast, the people closest to me didn't make it. They did not survive their cancer. And so it, It's taken a while for me to understand that, no, you can be diagnosed and it's not a death sentence tomorrow. People make it through this.
SPEAKER_03:Your doctors can say you have a 5% chance of living and you very well, Heidi and Tess, might be the two people. I think that's an excellent thing to say because when we talk about anxiety and that eye of the storm, we want people to first and foremost feel in control and in balance because in that very present moment, they are. Because you're right. It's never something that doesn't hurt. That scab is... that scar is always there, but you overcame it.
SPEAKER_01:And so,
SPEAKER_03:yeah. And even though your sister didn't, I'm happy that you still have a good outlook for yourself, even though there hasn't been good outlooks around you. Yeah.
SPEAKER_01:Well, and I think that was what was helpful when I first got diagnosed the first time, um, All the different people that came out of the woodwork to tell me, you know what? I had cancer. I had cancer 15 years ago and it was this and it was scary, but I'm right here. You're going to be all right. And I had numerous people that I had no idea had ever had cancer. I was in fact shocked by how many people had told me experiences like that. And those are very validating. And I think that's, for me, that's a huge point of the podcast is, okay, take a deep breath. And yes, it sucks. And it's horribly scary and whatever else. And yes, you're right. You may not make it. But guess what? Lots of people do. Yeah. And my mom said, Hyde, this is not 30 years ago. That's true. This is not 30 years. That's true,
SPEAKER_03:too. We're in. Yeah, it's 2021. And we have come so far from. Yes. When I was born in 89 or in the 90s and from when your sister passed away. You're right. It is different.
SPEAKER_01:I'm just listening to when you were born and thinking, yeah, I haven't even quite got your
SPEAKER_03:graduate from college. Isn't it so funny? But hey, look at, here we are now talking on a podcast together, which is just equally divine and amazing. And you know what, Heidi, if you and I help one person, one person, that's all we need to do. So like, I already know that you've helped more than one person and I sure hope I have too. And so.
SPEAKER_01:Well, you've even helped. I mean, I'm sure you have. a bunch, but you've helped me. You've helped. I'll tell you, I was listening. I listened to the first one you did with Annette and then the one you did with me about Macy with Don and Brian. Yeah. And I thought, yes, Heidi, you have things that you struggle with and Tess has different things that she struggles with. And some of the things you struggle with tests are things that are I don't know how, honestly, I don't know how I deal with them, but it gives me hope and strength and perspective to hear how you deal with them. And I think that's, I hope that's all I, it's funny because you use the word resilience and that's what I, that's part of my intro to my podcast. I want to share stories and experiences and expert advice with people to help them feel happier, more resilient and less stressed. That's it.
SPEAKER_03:Yeah, it's pretty incredible because whether someone's going through a cancer diagnosis or not, I think this will bring them a lot of perspective. And, you know, obviously you and I know, we both admit we don't know it all, but we know what we've been through and we know what's helped us and we know what's important to us. And so if we could just help people prioritize, I don't even want to tell people what order is most important. Neither do you. I know that.
SPEAKER_01:No, but you get to take the time to decide what's most important. Yes.
SPEAKER_03:No other time in your life, unless you're 85 or if you're from Heidi's family and there are hundreds laying on their deathbed finally going, oh, what do I want to do? What's important to me? As horrible as a physical health emergency is, It's pretty incredible that just as you having children, Heidi, kind of matured you and gave you a different perspective. This health care did that for me, too. This health issue did it for me, too. And sure, I'm not teaching two little kids at home right now. And I don't know that I want to be a mom anymore in this body because, well, I guess that's a story for another day. But I just don't know that I would
SPEAKER_01:But there are different considerations.
SPEAKER_03:Yes, because I don't know that I would be the mom I would want to be. And maybe God has a different purpose for me now with this. And I'm okay with that. I guess I'm becoming more okay with that. Do you want to wrap it up here, Heidi? It looks like we still needed to talk about tips and tricks and then bucket list items. But I think we touched on the other questions. Do you want to wrap that up so that our second episode, we can come up with new things or should we save those for next time? It's up
SPEAKER_01:on you. No, I mean, I think you, I think you gave a lot of your tips and tricks too. Well, you're sweet. No, no, I'm, I'm being totally honest and I just like, okay, besides writing a book, what else is on your bucket
SPEAKER_03:list? Um, I want to go back to Europe. I've been to Europe once. I want to go to the beach. I want to go on a cruise. I want to own an action track chair. Those are the things that are like... I don't
SPEAKER_01:even know what that is. It's like
SPEAKER_03:a snowmobile crossed with a four-wheeler, but you sit on it. It's like a power wheelchair that could go over downed trees. That's awesome. Oh, yeah. It's insane. It's like a tank chair. I'll send you a picture. Okay. And it would also be really cool to walk again, not even necessarily with my own God-given muscles, but with like an exoskeleton. I
SPEAKER_01:was wondering, can you support that? I
SPEAKER_03:think I could. I think I need to do some more stretching and I would like to get my weight down a little bit. Annette and I talked a little bit about how apparently there is a statistic, and now I'm going to blank on it, but about how men... leave their wives after they do this.
SPEAKER_01:Oh, I just looked into it. It was like 80%. So
SPEAKER_03:like 80% of men leave their wives if the wife is the one to get hurt. But then if a man gets hurt, it's much less. I just love that you go, uh-huh.
SPEAKER_01:Well, no, because- It's not surprising, right? I'm a-hunting the statistic. That's it. That's it. I'm just unhunting the statistic. That's it. But that's what you said, 80%. It was almost like the reverse for women. Yeah, and
SPEAKER_03:so it was a little different. But regardless, marriages were even more likely to not turn out if there was a disability. And oh my gosh, see, and this is the thing I hate about my chemo is it's like, what was I just going to tell you
SPEAKER_01:about that? Dude, I know like the short-term memory. Well, you were talking, were you talking about you and Tyler?
SPEAKER_03:Maybe. Were you going
SPEAKER_01:to talk about it?
SPEAKER_03:Maybe. I don't really know. Well, you said, oh, because we were talking about bucket list.
SPEAKER_01:And you were talking about your chair, your Rambo chair or whatever. Yeah. I
SPEAKER_03:mean, I guess I just, I, I want to experience more life too. Like I don't want to just stop here. I don't want to just stop growing here because I've grown so much, right? Like I want to keep growing, but I want to do it in a way that is most meaningful. And so I'm just really thankful to you too, for reaching out to me and again, being brave, starting this podcast journey, because look at where we are now. We're both doing it and that's pretty cool. And, um, as far as bucket list items, yeah, I would just say, for me, it's not even necessarily, you know, I know I listed a couple of things that I want to do, but for me, bucket list items, again, if I found out I was only going to live another month, I would ask Tyler to take a month off of his job and go to Minnesota. And I'd just be with my family and spend quality time with them or I'll go to Europe or I'll go to Europe together. Yes. Yes. Um, But yeah, I just, again, and then I'll just quick, let me just quick read off these tips and tricks because I have a list. Stretch, swim, do cardio. Whatever that looks like, whatever movement is good. Heidi, I know you feel the same way about that. You're talking about your lung health and needing to stay fit. I mean, before we went through health issues, we knew exercise was important. And so for sure, especially now as a woman who can't move her lower half, I have to stretch. If I don't sit cross-legged or in a diamond position, I'm not going to be able to do that in a year and a half. So I better be doing that every day. Um, I coming off of chemo, I used edible marijuana products that helped me significantly with.
SPEAKER_01:Oh yeah. I used the tincture
SPEAKER_03:huge difference. And you know what? I know people have a hard time like taking that or thinking it's beneficial, but coming from Heidi and myself, Heidi, you said you tried benzos and that was ended up just not doing well for you long term. The Oxy was not good for me long term. If you use the marijuana in a safe place and you aren't operating machinery and you're in the comfort of your own home and it's okay with your doctors, try it. Because I always tell people I would rather use something that God made himself than a bunch of people in a lab that didn't know how addictive something would be. Right. Um, the brat diet, I, with the chemo and I'm sure maybe with the, um, rate, what do you call the radiation? Gosh, I just totally couldn't even come up with that word. Um, sometimes your bowels get loose doing the brat diet, bananas, rice, applesauce and toast. And then also I got C diff a couple of times because the chemo just killed all the good bacteria in my gut. And so, Yes, probiotics, but also looking up home remedies for making barley water. You can put ginger in it or honey in it, and you literally just cook the barley. It's similar to rice, and then you drink the water after you take all the barley out. Do
SPEAKER_01:you need to let it ferment? I don't
SPEAKER_03:think so. I'm pretty sure you can drink it right away. And if you guys look it up online, I know people will find good information out about it, but I'll highlight that too, Heidi, and share it with you if... Oh, good. And I'll put it. Yeah. Um, but that's huge. Um, so yeah, those are my tips. I, I also will say, you know, one last thing really quick at the end here. I know this is getting long, but you know, I was, I was diagnosed in April and May and I didn't have my surgery until August. And so what is that? June, July, we'll say three months was in between. And there were people that also desperately wanted to save my soul and when they knew that i was a christian then they would say like okay well i want to save your back and your legs i i want to save i want to pray for your healing before surgery and and you know what sometimes that works people have meditated and prayed over lesions on their spine and they've gone away and i'm not saying that god can't bring a miracle because I know my God can, but I want to make sure people know that sometimes the reaction we get from someone who's never been through a health issue can be very different than say from Heidi, you or I. And so I remember feeling very frustrated one night and looking at my mom and saying, I'm just mad that people are even sending me this stuff because someone sent me like a six pound CD-ROM album thing. It was literally about just simply God helping you walk again. You're like,
SPEAKER_01:okay, that's not my reality right now. That's so
SPEAKER_03:unrelated to a cancer taking over. It's
SPEAKER_01:really hard to acknowledge the kindness and the thought behind it when you're in the middle of
SPEAKER_03:it. I was thankful for it. I felt sad that the people who gave it to me didn't realize that like, it was just, I don't know. I don't want to say distasteful because that sounds mean, but you know what I
SPEAKER_01:mean? It's insensitive. They mean well, but yeah, because
SPEAKER_03:it's like, did the, did these people not think that I hadn't prayed already hard enough for God to heal me? Like I have stayed up nights praying for God to heal me. Right. So
SPEAKER_01:did my sister. So did all my whole family.
SPEAKER_03:And so, I don't know really even what I'm trying to say here, but I know you get it. Well,
SPEAKER_01:yeah, it's like, because what's going to happen, you know, what's going to happen is going to happen. Like, I totally believe God has a plan, but I don't know that plan. I'm not omniscient and omnipotent. And sometimes we are allowed to experience things. I don't think God causes all the bad things. People say that all the time. I'm like, no, I don't believe that. But I think we are subject to physical bodies that have things that go wrong. And sometimes they get healed, like in my case, like in your case. And sometimes they don't. And it doesn't mean anybody's any less faithful or valuable or whatever if it doesn't work out the way we in our finite minds think it should.
SPEAKER_03:Yes. And then what a perfect way for you to end this episode because how much better can we love those around us the way Jesus would love people around him if we focused more on just being accepting of wherever people are at and not pushing our ideas of what's best for them on them. Yeah.
SPEAKER_01:Yeah. I think that's a perfect way to end it. And I want to do more of these with you because I've so enjoyed this. You're just delightful. Well, I think
SPEAKER_03:you're delightful, and thank you. I am a confident person, and I am a hopeful person, but I also know that I can talk a lot. My mom would say, you can really talk forever. But Tess, I think you've got a lot to say. Yeah, well, I do. I do have a lot to say. And I don't even really know how to say half of this stuff, which is why for me too, a book is just like, oh my gosh, I can't even get my head on straight. Like I can barely handle making my outlines without having them be too all over the place. And so... I do have a lot to say, Heidi, and I know you do too. And I'm looking forward to more conversations. If not, now people are familiar with us both and you and I are familiar with each other. And so, yeah, we can start an outline and talk more in the coming days. So thank you so much for having me on your podcast, Life, Cancer, etc.,
SPEAKER_01:Well, and thanks for having me on Push Diaries podcast too. I've been looking back over the work you've done over the last year and I think it's pretty incredible. So thanks for being willing to do this. And thanks for not being like, who is this freak? No, you're no
SPEAKER_03:freak. Are you kidding? No. I want to hear more people's stories and I know you do too. So if anybody has anything they want to say to either of us or want to submit questions, please do because Heidi can make a list and we can get back on here and talk about whatever we want. That sounds great. Before you go, tell us where you're at as far as like your, your next scans that are coming up or what are you looking, looking at
SPEAKER_01:as far as. I've got, I've got PET scans coming up in about a month.
SPEAKER_03:Well, I've
SPEAKER_01:got a consult next
SPEAKER_03:week. Keep us all posted on how those go. And I'll be praying for you all the way from Michigan.
SPEAKER_01:Thank you. And I'll be praying for you too. So your thing is July, right? Yeah, not
SPEAKER_03:till July. And I'll be in touch once that comes around too. You'll definitely be hearing about it because that'll be a... big one for me you know a whole year it's like I really have I think COVID has helped distract me and this podcast just not over worrying about it because there were days and Tyler's so helpful too you know sometimes I'm like oh my back hurts more and he's like oh it's because you're getting your period or oh it's because you haven't had your midday medication you like oh you didn't have your gabapentin and I'm like oh crap I didn't and so it is it's just it's nice to have people around you that know what you worry about to go, Oh, stop it. Like it might be okay. Try not to go there because.
SPEAKER_01:Yeah. Okay. We'll say, or it could just be because you woke up at 3am and didn't get back to sleep. I'm like, Oh, good point.
SPEAKER_03:Yeah. You're like, there's some truth to that. Well, Heidi, thank you for talking to me for a stink in two hours.
SPEAKER_01:But it was, it was great. It was great. I'm really grateful that I got to spend, as she put it, two stinking hours talking with Tess Fole. She's an amazing example of adaptability and resilience and positive thinking. And I'm grateful that we get to collaborate in the future and that I get to know her better. This week, as you go around the world, try to do something nice for somebody else to make their day just a Then look for the good, count your blessings, and make it a great week. You can check out Tess's podcast at Push Diaries Podcast, and I'll put the link in the show notes. Thanks for listening.