Sydney Eye Podcast | @CabreraMarie
Sydney Eye Podcast | @CabreraMarie
Herpes Simplex Keratitis
Use Left/Right to seek, Home/End to jump to start or end. Hold shift to jump forward or backward.
Did you know that a corneal infection caused by herpes simplex virus is one of the main causes of blindness in developed countries?
Corneal specialist, Prof Stephanie Watson chats with Dr. Maria Cabrera about how to identify and prevent this infection.
If you have any questions, comments or suggestions please send them to sydeyepodcast@gmail.com
The Transcript is available in the 'Transcript' tab on this page.
Closed captioning for this episode can be also found on YouTube --> HERE
Don't forget to listen to our previous episodes -->
Ep2: Antimicrobial resistance in corneal infections
Ep1: Corneal infection and contact lenses
Connect with us on Twitter:
Dr Maria Cabrera: @CabreraMarie,
Prof Stephanie Watson: @profswatson,
Corneal Research Group, Save Sight Institute, University of Sydney: @cornealresearch
using #Sydeyepod
Music provided by: Energized morning by Airae
Link: https://www.epidemicsound.com/track/xF2ADhIuB9
Maria Cabrera: Have you heard that a corneal infection caused by herpes simplex virus is one of the main causes of blindness in developed countries?
Did you know that nine in ten adults have been exposed to herpes simplex virus?
Did you know that one in five people after an ocular herpes simplex infection can develop a chronic infection with the risk of blindness?
By the end of this podcast, you’ll know…
· What herpes simplex keratitis is;
· How to identify this infection, and
· What to do to prevent this infection.
First, I will give a brief introduction about corneal infection caused by herpes simplex virus. Next, I will chat with Prof Stephanie Watson, a corneal specialist and the head of the Corneal Research Group at the University of Sydney, Save Sight Institute, and the Head of the Corneal Unit at the Sydney Eye Hospital, who will tell us how to identify a corneal infection caused by this virus and will give us some recommendations on how to prevent this infection. And later, we will explore the research on the treatment for herpes simplex keratitis.
I am Maria Cabrera-Aguas. A Researcher at the University of Sydney, Save Sight Institute. Welcome to the Sydney Eye podcast!
Today, we are going to talk about herpes simplex keratitis. Remember that a corneal infection is also known as ‘keratitis’. There are two types of herpes simplex virus: type 1 which causes infections in the face for example the common “cold sores” around the lips and nose; and type 2 which causes infections in the genital area.
An individual usually is infected by the herpes simplex virus during childhood. Only 1 in 100 patients present with signs of ocular infection. The herpes simplex virus type 1 is transmitted via direct contact with sores and saliva of a patient with the infection. The ocular infection generally manifests with small blisters on the eyelids or surrounding skin, red eye, and lymph nodes in front of the ear within a month after the infection.
After the initial infection, the herpes simplex becomes inactive in the body. Recurrent corneal infections occur when the virus is reactivated and is transported down the nerves infecting the cornea again. Reactivation can be triggered by trauma, fever, or environmental factors such as windy days or sunburn. Recurrent infection can affect the eyelids, conjunctiva, cornea, or retina.
Herpes simplex keratitis is an important cause of blindness in developed countries. One in five people who have had ocular herpes simplex virus infection are at risk of having recurrent infections which may cause scarring in the cornea leading to blindness.
1.5 million of new cases of herpes simplex keratitis were estimated in 2012 worldwide. Patients require frequent visits to an eye doctor resulting in significant loss of time at work and reduced productivity. Patients see an eye doctor on average four times during the first episode and six times when the infection recurs. Corneal transplantation may be required when multiple recurrences of herpes simplex keratitis cause corneal damage. Over 1,000 surgeries are performed annually in the United States in patients with herpes simplex keratitis. In Australia, 1100 corneal grafts have been performed due to herpetic eye disease since 1985.
Now, let’s welcome Prof Watson, a corneal specialist and the head of the Corneal Research Group at the University of Sydney, Save Sight Institute, and the Head of the Corneal Unit at the Sydney Eye Hospital. We are going to chat about how to identify this infection and what we can do to prevent it.
Thank you, Prof Watson for joining us again in our show today. Welcome!
Stephanie Watson: Thank you. It is nice to be here.
Maria Cabrera: how often do you see patients with a corneal infection caused by herpes simplex virus?
Stephanie Watson: herpes simplex keratitis is the commonest cause of corneal blindness in developed world. So, every day that I am in practice I see at least one patient with herpes simplex keratitis. It is pretty common. When we did an audit at our corneal clinics at the Sydney Eye Hospital, we found that herpes simplex keratitis was the second most common reason of patients to visit there.
Maria Cabrera: Well, it seems quite a common ocular infection then. What type of patient usually has this condition? Young, old, with any medical or ocular history?
Stephanie Watson: Well, it is interesting, almost any age of patient can have or had had herpes simplex keratitis. It starts as an acute condition and then you can get a chronic form that can go for many years. So, someone might come in and visit in their sixties who actually had their first episode in their twenties. I have also seen children with herpes simplex keratitis. So, it can affect all ages. But overtime people might get more and more episodes and then might become a chronic condition.
Maria Cabrera: So, listeners this is a key point, any patient, child, or adult, can have herpes simplex keratitis. Then Prof Watson, what symptoms do patients or parents need to watch out for?
Stephanie Watson: If they get a red eye, it is not resolving quickly, and they are light sensitive, or the vision goes down. It is more common in patients that have cold sores on their lips, and those cold sores caused by the herpes virus and it is the same form of the virus that causes cold sores on the lips as it does on the eye.
Maria Cabrera: When does a patient with a red eye need to see a doctor? How many days after the onset of symptoms?
Stephanie Watson: look, a red eye that is not getting any better probably get it seen too quick than a week, you know if it is not going away after a day or two because it can also be very serious causes of red eye, I mean including herpes simplex. So, I would recommend that a red eye that is not getting better after a day or two, have that eye checked. If there is pain, have it checked sooner, if the vision is down, have it checked very soon.
Maria Cabrera: Why do you think people should know about herpes simplex keratitis?
Stephanie Watson: it is important because it is really common and can lead to blindness. And once you have herpes simplex, it can come back again and over time it can cause more and more scarring on the cornea and therefore more and more vision loss. It is important patients are aware or know that they have herpes simplex keratitis, so if they get a red eye again, they can come quickly so they do not lose more sight from scarring and vascularisation of the cornea and they can get it treated properly. It is important that patients know about the condition so if they do get a red eye, they can consider it particularly if they got a cold sore.
Maria Cabrera: Now, let’s talk about treatment, what treatments are available for this infection? How is usually treated?
Stephanie Watson: the main treatment is particularly at first presentation is antiviral treatments. And these inhibit the replication of the virus, so the condition can resolve faster. If it is a recurrent condition as well as the antivirals, you might also need to use some topical steroids. The herpes virus when it causes keratitis causes inflammation and vascularisation and steroids can have a role in resolving the inflammation and vascularization to prevent further vision loss. But if you are using steroids you may need to monitor them closely, steroids can put the pressure up in the eye, they can cause cataract and if not giving with the appropriate antivirals you can get corneal melting. Rarely in herpes simplex keratitis the cornea maybe is so badly affected that melts away and then you can get what it’s call perforation where there is a hole in the eye and this would need urgent repair. Now there is a number of ways that we repair corneas with herpes that have perforations. If it is a small one you may just be able to treat it with what we call ‘bandage contact lens’ which is a contact lens that goes on and it’s used literally as a band-aid or bandage. If the hole is bigger around two to three millimetres, you can do then what it is called the ‘glueing’, we have almost a super glue in the eye, you put on and that can stop the leak, but if it is bigger again you probably need to do a corneal graft. We use tissue donated and we stitch this into the eye to heal the leak. There is range of treatments patients might need depending on how severe the herpes is and what stage it is.
Maria Cabrera: indeed, this infection can cause severe complications needing even a corneal transplantation. Can the patients do anything to prevent this condition?
Stephanie Watson: sometimes it is thought that being run down or fatigue or being immunosuppressed actually increase the risk of herpes virus manifesting itself as a disease that is in the eye or in the lips, because most of us actually have been exposed to the herpes virus and if you look at the blood of people, you know, let’s say when there are sixty, the majority of us actually have antibodies to herpes simplex indicating our previous exposure. Around 1% of population manifests herpes as a disease. We think that maybe immunosuppression such as if you have a kidney transplant might make you more prone to have herpes simplex keratitis. Actually, if you have a corneal graft can also increase your risk and this is probably due to immunosuppression use steroids. Patients are at risk maybe put on to oral antivirals to help prevent recurrences. There is very limited evidence but there has been speculation that a diet rich in lysine and low in arginine may have some role in reducing episodes of herpes simplex but this is, this is still remains to be proven in larger studies. So, I think in summary, take care of yourself, have a fit and healthy lifestyle, if you are on immunosuppression, find if you need to be on antiviral prophylaxis and maybe just consider whether you diet is ideal. This is what to can do to prevent episodes.
Maria Cabrera: Well, Prof Watson, this was very informative, thank you so much for being on today’s episode.
Stephanie Watson: Thank you. It was a pleasure!
More on herpes simplex keratitis up next…
But first, we have a question for you, the listeners. Have you had a corneal infection caused by herpes simplex virus before? If so, how was your treatment? Were you treated as an out-patient or admitted in a hospital? What medications were you prescribed?
Email us at sydeyepodcast@gmail.com or share on Twitter with the hashtag sydeyepod, that’s Hashtag S-Y-D-E-Y-E-P-O-D.
Now, more on the research of treatments for herpes simplex keratitis
The cornea has three layers: the epithelium, the stroma and the endothelium. When the herpes simplex virus infects each layer of the cornea, the infection manifests differently. The appropriate therapy for each type of keratitis depends on the correct diagnosis made at medical examination and whether they had a previous infection. Sometimes doctors can perform a swab on the eye to detect the virus.
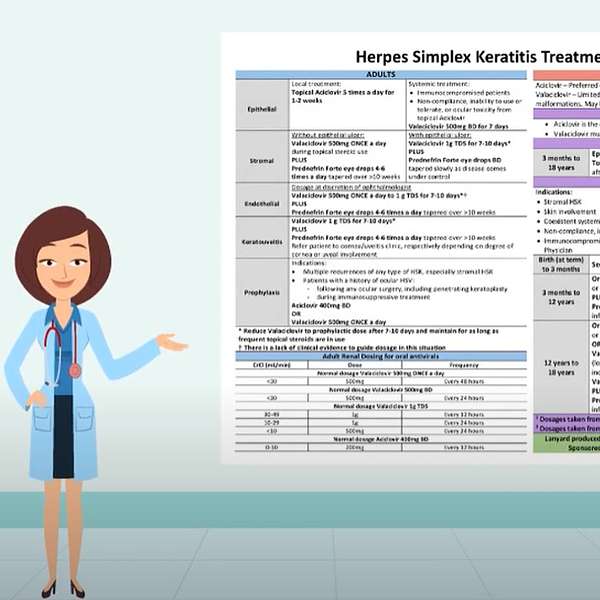
At the Sydney Eye Hospital, Prof Watson and I led a group of corneal and uveitis specialists and pharmacists to develop, implement and evaluate a clinical guideline for the treatment of this condition. In 2014, we found that there was a diverse range of initial therapies given in 73% of clinicians prescribing the initial anti-viral therapy according with the recommendations of clinical trials. Next, we created the local guideline based on the clinical studies and available antivirals in Australia. We distributed the guidelines through lanyard cards, put up posters in consultation rooms in out-patient clinics and in the emergency department, sent a pdf document via email and uploaded the guidelines on the hospital intranet and on the Save Sight Institute website. This guideline outlines the initial therapy for epithelial keratitis, stromal keratitis with and without ulceration, endothelial keratitis, keratouveitis, prophylactic therapy, adult renal dosing for oral antivirals, recommendations for pregnancy and for children. We have also sent out the guideline to clinicians who have requested them for their practice.
We also evaluated the uptake of the guideline among clinicians. We did a medical records audit and ran a survey. Most of the clinicians were aware of the guidelines and used them at least twice a week. There was an increase from 73% to 80% of clinicians following the treatment recommendations for herpes simplex keratitis after implementation of the guidelines.
I have also created two videos about herpes simplex keratitis which are available on YouTube. You can find the first video as ‘Educational video to support diagnosis of herpes simplex keratitis’. In this video, I highlight the signs of each type of keratitis for clinicians to correctly identify the type of keratitis which will help them to prescribe the appropriate therapy. You can find the second video as ‘Educational video to support the treatment of herpes simplex keratitis’. In this video, I explained the treatment guideline.
In summary, herpes simplex keratitis is a corneal infection caused by the herpes simplex virus. It is one of the main causes of blindness in developed countries. Individuals usually get the virus in the childhood but only 1% develop ocular infections.
Children or adults can have keratitis. It usually presents with a red eye associated with cold sores on the lips. If you also present pain in the eye or loss of vision, please see an eye doctor immediately. Recurrent episodes may cause scarring on the cornea leading to blindness.
To prevent recurrent episodes, have a healthy lifestyle and if you have any immunosuppressant condition such as a previous organ transplant including a corneal transplant, or use of chronic steroids or immunosuppressant medications, or any previous ocular surgery; you may need oral antivirals to prevent recurrent episodes. Consult with your doctor.
I am Maria Cabrera-Aguas, thanks for joining me today in the third episode of the Sydney Eye podcast.
If you have any questions, comments or suggestions please send them to sydeyepodcast@gmail.com and connect with us on Twitter @CabreraMarie, it’s
C-A-B-R-E-R-A-M-A-R-I-E or @cornealresearch using the hashtag S-Y-D-E-Y-E-P-O-D. Until next time. Bye!