I Need Blue
I Need Blue holds space for survivors to speak truth, reclaim power, and rise. These stories are lived. They carry scars and strength, pain and rebuilding, and the steady reminder that nobody heals alone. I survived, too, and this space was born to help you feel seen, supported, and guided toward real resources and real hope.
I Need Blue
Addressing Compassion Fatigue in First Responders: Strategies for Mental Health Maintenance
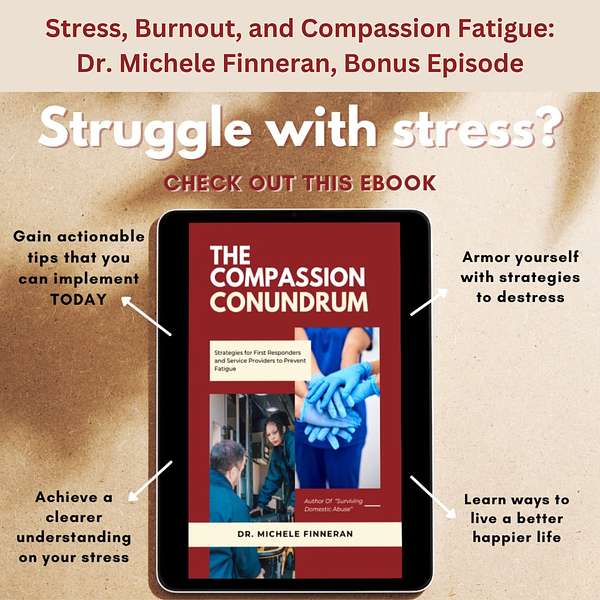
In this insightful episode, Dr. Michele Finneran, a leading psychotherapist and mental health advocate, explores the mental toll of compassion fatigue faced by first responders, healthcare providers, counselors, and others in service professions. She shares valuable strategies from her book, The Compassionate Conundrum: Strategies for First Responders and Service Providers to Prevent Fatigue, offering seven practical self-care tips that help professionals balance their commitment to others while maintaining their own well-being.
Dr. Finneran also discusses the importance of destigmatizing mental health in first responder communities and highlights the role of peer-to-peer support groups. Additionally, we explore the impact of secondary trauma on the families of service providers and how they can also benefit from mental health support. This episode provides essential insights for anyone in service professions to safeguard their mental health and prevent burnout. Tune in for actionable advice on staying resilient while caring for others.
Connect with Dr. Michele Finneran:
https://www.veccandassociates.com/
Connect with Jen:
I Need Blue now has a new home at The Healing in Sharing! Visit thehealinginsharing.com to explore Round Chair Conversations, all relevant I Need Blue content, and ways to support the mission of sharing stories that inspire hope and resilience.
By sharing the hidden lines of our stories, we remind each other we are not alone — together, we step out of hiding and into healing.
Instagram: @ineedbluepodcast
YouTube: https://www.youtube.com/@ineedblue
Apple Podcasts: Listen & Subscribe
YouTube: https://www.youtube.com/@TheHealingInSharing11
Memoir: Why I Survived, by Jennifer Lee on Amazon
The background music is written, performed and produced exclusively by Char Good.
https://chargood.com/home
Everyone has a story. They just don't always have a place to share it. Welcome back. This is Jen Lee, creator and host of I Need Blue podcast. True Crime to True Life. As a survivor of arm dropery and abduction, I understand the trauma and triggers survivors experience Knowing this and through my powerful podcast, I offer survivors a safe place to share their lived experiences. Survivors need blue to feel they belong, they are loved, understood and my favorite empowered. Please note I Need Blue does contain sensitive topics which could be triggering. Please seek help if needed and remember you always come first. I Need Blue episodes can be found on Apple Podcast, Spotify and many listening platforms, including my website, wwwineedbluenet. I would like to thank Char Good, the talented violinist who composed and performed this opening music. You can find information about Char Good on my website. As always, thank you for listening.
Speaker 1:Let's begin today's episode. Get ready to be enthralled by our special guest, Dr Michelle Finneran. She's an author, a psychotherapist and a passionate advocate for mental health. Some of you may remember her from a previous appearance on I Need Blue, where she shared her invaluable insights on supporting the survivors of the Parkland School shooting. I'll include the link in our show notes if you missed that episode. Today, I'm delighted to reconnect with Michelle as we delve into a vital topic the well-being of our first responders. Her latest book, the Compassionate Condundrum Strategies for First Responders and Service Providers to Prevent Fatigue, is a must read. And here's the fascinating twist you don't need to be a first responder to benefit from these insights. Many of these strategies apply to our everyday lives. As a podcast dedicated to providing valuable resources, this episode is your chance to gain a deep understanding of stress, burnout and compassion fatigue. Michelle is here to enlighten us and we are truly grateful for her presence. Welcome back, Michelle, and thank you for being my special guest on the I Need Blue podcast.
Speaker 2:Thank you, jen. I'm so happy to be back it's been a minute and I'm so happy to come back again on your important podcast. I think it's very important that you have podcasts like this to educate, inform and raise awareness, so thank you for having me back.
Speaker 1:Absolutely, and I appreciate you and everything that you do as well to help people in their healing journey. I want to start with this question. The title of your book is called the Compassion Condundrum. Tell me why you picked that title?
Speaker 2:Me and my team were talking about a kind of a catchy title that would stick in people's mind A condundrum. We don't hear very often. Like you mentioned, it's an interesting combination of words the compassion condundrum because when you think of a condundrum you're almost like in a crisis situation, like you're frazzled, you know you're struggling as a first responder or a service provider or healthcare professional. A lot of times we feel in condundrum because we're outpouring so much compassion.
Speaker 1:Absolutely Like for me. I'm an empath, so I feel that individual's emotions, and so for me it was really finding that balance between being able to relate to my guest or my friend, my family member, but then also make sure I have my boundaries.
Speaker 2:Yeah, and I did an interview we talked about the mentality of first responders, always in the old mentality, old school mentality of always putting others first, others first. And so the importance here in this compassionate condundrum, is, you know, it's almost like the airplane simulation where you take your mask down, you put it on yourself first and you put it on another person. This first responder really has to value and put themselves first. And service providers have to put themselves first and make sure that their mental health and their physical health is on point before even attempting to try to help anybody else in an effective way. So that's why first responders old mentality is we're putting everybody first, because this is just what we do. But no, that's the old way of thinking. The new way of thinking is like first responders have to put themselves first.
Speaker 1:Absolutely. You know, when you first started talking about that, I had a visual the putting on your mask of being a parent, and you put it, that mask on yourself first and then you put it on your child. But what's very different about being a parent and being a first responder is within that our first responders see situations that many of us could never possibly imagine. And that's where your ebook, the compassion conundrum I have to say conundrum slow, because it's almost like a tongue twister. It's almost like a tongue twister for me, but I've gotten it out.
Speaker 2:It's hard for me to even spell. I can't even spell it right. I get it confused. I know it's very, it's funny.
Speaker 1:I love it, though it's perfect. It's like a conversation piece in itself, yeah, and that's so important because this is a conversation that needs to be had, absolutely, and I'm so glad that you wrote this book. Let's talk a little bit, then, about stress, burnout, compassion, fatigue, how they're the same, how they're the same, how they're different, how they relate to first responders, how they relate to people like you and me. There's so much to unpack here, yeah, and I can't wait to get started, absolutely.
Speaker 2:So in the book we define stress, the definitions and the symptoms and the cinematology of regarding stress and burnout. You know, in the research and literature which is all this book is based on literature and research and academia is that there's no real clear definition. But the most popular definition I found as a physical and mental, emotional strain up to our tension that stress incurs and the condition of feeling experience when a person perceives that the demands exceed the personal and social resources that the individual is able to mobilize. So that is part of stress. That's kind of like the most popular definitions. It varies but this is what I found the research to be the most sub definitive with when it comes to stress.
Speaker 2:And then we talk about, like E stress, which is motivating stress, which is positive stress, and we talk about D stress, which is paralyzing, and negative stress and the feelings of being overwhelmed. Which defense mechanisms are these fight, flight and freeze responses that we talk about when we feel stress and it manifests? I know I know a lot of people that manifests in different ways. Stress can manifest within the body, it stores in the body, it has physical manifestations. That is part of stress.
Speaker 1:You're right, everybody handles stress differently. Something that might stress me out might not stress you out, right, exactly the fight, flight or freeze response Boy. Have I felt that Absolutely. In regards to therapy, being able to get yourself out of that fight, flight or freeze can be tough. It is yeah For me. I think there are times where my body has stayed in it and I didn't even realize that it was in it. The other is, yeah, the paralyzing stress, the negative stress. Would that be comparable to like depression?
Speaker 2:Yeah, Usually it can go to one or two ways. It can reach a level when you're that overwhelmed, as stressed, it can reach like paralyzing anxiety and anxiety. It can turn into an anxiety issue and it can also turn into a depressive state. In the book it talks about not just that, not just psychological manifestations of stress, but also physical manifestations as well. The goal is that therapeutically, before you're going down a paralyzing state, is to catch it early on. It's early detection, one of the key signs before we're going down a rabbit hole. Once you're going down a rabbit hole, therapeutically it's harder to come back to surface. If you have early detection and you have early awareness and I talk about how to detect that in the book that is going to be key to helping the transition smoother and out before going deeper into a dark place. That early detection awareness is super helpful therapeutically before it gets to a point at a control point.
Speaker 1:Absolutely Basically, understanding your triggers yes, yes and knowing how they feel in your body. I am so glad that that is in your book, because, to me, if you don't know your triggers which is step one right then how do you figure out how to cope, yes, and then not end up feeling that way again? You know, we're 27 days away from Christmas and people experience that seasonal fatigue.
Speaker 2:Yes.
Speaker 1:How does that fit into this topic of stress?
Speaker 2:You know, not just seasonal fatigue but financial fatigue. I'm hearing a lot of that coming up in my sessions. A lot of people around this time have a lot. They feel like they can't do as much as they want to do monetarily for their kids and that really stresses a lot of parents out. When that becomes a part of the family dynamic it's very challenging to overcome and we know we're having these conversations and sessions right now about financial stress Because everything not just not even with Christmas coming or holidays coming just with everything just skyrocketing up. Everything is so expensive and people now closer to the holidays is becoming more and more concerned.
Speaker 1:Absolutely. And a lot of times we place so many expectations on ourselves yes, that we're expected to do this or do that and a lot of times things are out of our control, like right now, the cost of groceries we can't control if they go up the cost of gas. So, like you said, that financial stress, it fluctuates, and so many of those factors we don't control. We don't control.
Speaker 2:But there is things that we can control. Is the feelings taken away from it Like I have a lot of parents like having parental guilt. You know, when we start doing that, especially with parents that have young kids, you know we start to lose sight of the essence of what Christmas is really about?
Speaker 1:Yes, thank you so much for sharing, and now this topic is going to lead us into burnout. Can you tell us a little about that?
Speaker 2:So, yes, burnout is the emotional and physical exhaustion of excessive, prolonged stress. So stress is one level and burnout is a higher severity of level than stress. And when we think about burnout we usually think about job burnout. Burnout can happen professionally and personally. It's definitely very much so part of ability. When you're unable to meet high demands, it definitely zaps energy levels, it threatens your job, it threatens your health, it threatens your relationship and it's a feeling of not being enough, not doing enough, feeling empty and devoid of motivation and beyond. I think that burnout is another level of stress prolonged stress, because stress can happen immediately and can not last that long, but burnout is a prolonged stress.
Speaker 1:It's more threatening. Yes and the first responders. They're more prone to the burnout.
Speaker 2:They are. They are more prone to burnout, but they're even more prone to compassion fatigue, more so than any other profession.
Speaker 1:Let's move on, then, to the compassion fatigue.
Speaker 2:So compassion fatigue I love this term because I experienced compassion fatigue during COVID and I'm still experiencing a little bit of the aftermath of it as a therapist and anybody who is a first responder or a service provider, people that I help, people who help other people so that's the niche of my practice and people that help other people prior to focusing on their own needs, are much more prone to compassion fatigue.
Speaker 2:Whether you're a service provider, whether you're a first responder, whatever the case may be, the difference is it's different type of exhaustion than burnout, than stress, and it's continuously kind of giving of yourself, feeling depleted. But the one thing that happens in compassion fatigue is feeling completely apathetic and it's hard to be a first responder or a caregiver or a service provider and provide effective services when you're feeling apathy. Apathy is like the act of not caring. So that's why compassion fatigue is the negative costs of caring. You're outpouring so much as a first responder and service provider that you're feeling so depleted that the care now is jeopardized because there's a lack of compassion. So that's why compassion fatigue is a term coined, first coined in the nursing industry. Charles Fiddley coined the term and he coined it because it's not only a physical and emotional psychological impact of helping others. It also has to do with secondary traumatic stress, trauma that only first responders see, only service providers here and see. That's another higher severity element to compassion fatigue.
Speaker 1:You know, until we started to have this conversation, I was not familiar with compassion fatigue, so you have educated me so much already and I know that there are people listening that after you just described it are like, oh wait, that's me. Yeah, I understand now. That's what's going on.
Speaker 2:Just so you know the reason why I'm so passionate about this. This is because I experienced it myself as a clinician, but I also because my niche in my private practice is helping people that help other people first responders and service providers mainly that I help them to help their staff, their clientele, their patients, the community to become more effective one giving care. So I saw on both sides of the coin one experiencing it personally and one helping people out professionally.
Speaker 1:Can you share if you're comfortable with your experience then, and how you have helped yourself get through this compassion fatigue?
Speaker 2:Honestly, jen. In the book it's outlined seven no-brainer strategies that first responders and service providers must do there, must do, and so there's seven things outline. I do an eclectic of things. I realized that I needed to do something to help myself, and not nothing maladaptive, not these vices that are set up to help short term but then become an additional issue, like the vices that we talk about excessive sex, excessive gambling, excessive drinking, excessive drug use, marijuana use, all this stuff that we use in excess to numb to deal in the short term, and those are all maladaptive. They're all vices. So instead of leaning into those, as a therapist I know not to do that, but I'm also a person as well. So I decided to have a eclectic, different type of eclectic toolbox. For instance, I wake up early in the morning and before I start my day, I say a prayer. I make a prayer every Sunday for the week and I say it out loud before I start my day, every single day, with a cup of coffee. One cup, one cup of coffee. I don't have one cup of coffee, I can't even say a sentence. So I have one cup of coffee and my prayer. That's the first thing. Then I go for an hour walk every single day, even on the weekends. I go for a walk every single day and I have a meditative walk with myself, meaning I can think about everything. I usually think about my week because I don't want to get overwhelmed and put myself in anxiety patterns. So I think about just the week ahead, I think about my day, I think about what I'm going to wear, what I'm going to eat, I think about how I'm going to hide, how I want the day to look for me. So it's a premeditative walk with self in nature, only in nature, and then I start my day. I start my day and that sets my day up for success Doing those things I think in AM routine. A PM routine is super helpful. That AM routine always sets me up for success. And then I go through my day and I have a pretty long day On. Sundays is my day, my self care day. Sundays is when I do my reading. Sundays is when I write out my devotional. Sunday is when I meal prep. Sunday is when I take care of my hygiene. I wash my hair, I shave, you know stuff like that. Sundays is my day. For me, it's my self care day If I provide mental health for other people, try to provide good mental health for people.
Speaker 2:I got to be walking the walk. I also have to have good mental health. I also have a therapist. I have a therapist to help me. I have a business coach that helps with my business. I have professionals that help me when I may need the help. I have therapist friends. I have formal and informal supports. I have a good social network. I have a loving family. Those are all very important things to put in place. So you are completely, 100% balanced when you are trying to give care, whether it be a first responder or a service provider or just caring for your parents, an older adult Very important to have a clinic. You can't just have one thing. You have to have a multitude of things because there's so much, so much struggle. The people are just really struggling and one thing is not going to be an one-all fix-all. You have to have a toolbox of things.
Speaker 1:I love that. Different avenues For you. You found creating that routine in your morning to be beneficial, being intentional about your self care and putting yourself first and allowing yourself to put yourself first, because a lot of people the helpers, they don't know how to put themselves first.
Speaker 1:They're not trained, they're not trained to Correct, correct. I'm listening to you and you give me hope. I don't have the compassion fatigue at the moment, but my heart is filling up and I was like gosh. I feel hope and I know when other people listen to this, your passion, your authenticity, your I've been there comes through in your voice, in your words and your recommendations. So thank you, you're welcome. Thank you for recognizing Absolutely. You know we talked about routine and for a first responder. Every morning they walk out that door. They don't have a routine because every call is different. They don't know what they're going to walk into Exactly. How do you help someone with that type of a schedule, if you will.
Speaker 2:Yes, having some type of personal routine may not you may not be have a structure professionally, because you absolutely don't know what kind of call you're going to get, or how you're going to be jeopardized, or what your safety is or what you're grieving to see. You don't. You don't have that predictability. So you have to be prepared for just about anything as a first responder, and so in your personal life, you can you have more control. You do have a little bit more control, though in places where you do have more control, utilize that, like in your personal life, in order to be as much as you can, professionally, mentally, prepared for the unknown.
Speaker 1:I think that's great advice Control what you can control. I think we would both agree that there is more of the mental health, the coping skills training needed for our first responders and 911 dispatchers, and nurses and caregivers.
Speaker 2:Absolutely, and it really falls on progressive cities and municipalities and hospitals and organizations to really take care of their employees mental health, and the way a city or a company can do that is providing an employee assistance program through their HR department where they are getting free counseling. Insurance is good for their mental health. But the company that their organization, the city, the hospitals can set up, understanding that a day off shouldn't be explained as to why a service provider or first responder needs to take a day off. They just do because of the field that they work in. So it's having progressive cities, municipalities and organizations and hospitals and administrative people in position of power.
Speaker 2:You really understand that this is a really big thing and it just trickles down atop. It can really benefit and I've seen some cities in my area that are real progressive and their, their employees, feel very much well taken care of and they do a better job because of it. So and I see other cities that don't they don't. The burnout rate and capacity past fatigue is higher. It has to start. It starts for I could start within with your own individual work, but collectively and collectively and macro level it needs to start with the higher ups in these municipalities and needs to start higher up in these hospital administrations. It needs to start higher up and it have a trickle down effect, so the employee feels that they're worthy and they're valued Absolutely and, like you said, it starts at the top.
Speaker 1:They're the ones that are the decision makers that can decide hey, we need to implement this. There is a need. I think that recently there has been more of a spotlight put on the mental health of our first responder. Certainly not enough.
Speaker 2:No.
Speaker 1:The conversation has started. Oh my gosh, this book is going to be a great asset as well, especially in those areas where nobody's ever talked about it. Now you're like here, here's a resource, here's a tool like this is really what's going on and here's how we can help. Many times for our first responders, they're afraid to ask for help Absolutely yes because they're afraid of losing their job. They're afraid of losing their job.
Speaker 2:They're afraid of personally looking weak. There's a lot of fear and a lot of still stigma specifically with this, with this professional niche, a lot of stigma that's placed on them and that's why peer-to-peer counseling is very important too, for first responders is because they lean into each other more than they would a professional intervention. So that's why peer-to-peer support groups and peer-to-peer people that know exactly like what they're feeling in the moment, what they're feeling. It is important to also debunking and destigmatizing mental health in general, not just with first responders or service providers that think that going to a mental health professional makes you look vulnerable and weak is really debunking that myth. Actually, it's a sign of strength, it's a sign of courage and making that call is always probably the biggest, most anxiety-provoking thing ever.
Speaker 2:And stepping into the first session is having a therapist who will take all calls, not just, you know, having just go return the calls actually and knowing that the first call is the hardest call, and therapists also realizing that the first session is the most anxiety-provoking session, and having compassion in those areas. If I can't, jen, if I can't take on clients, because I have a high caseload, because this year I had to hire somebody to help me in my group practice, which has been amazing. She's been super amazing and super helpful with me and helping me unload some of the client numbers. But if I can't help them, I still call them back. I don't care, because that call is the hardest call to make. Even if I can't help them, I can figure out a way to figure out some way in which to give them something to leave with so they don't feel helpless or hopeless, because that call is the hardest call to make.
Speaker 1:Okay. So that puts a smile on my face because you are so right taking that first step and for many it is picking up the phone and making that phone call and I can't imagine doing that and not getting that call back. I'm so glad that you stress the importance of that, because as a therapist you're busy. Like you said, your workload is heavy. I'm sure everybody's workload is heavy, but at least acknowledge their courage and their strength to call and then provide them another resource, like you did. You have somebody else now there to take on other cases when you have a heavy workload. That is great advice.
Speaker 2:Yeah, as a business owner, you have to constantly assess your business and the needs of the business and the needs of the people, especially an entrepreneur that provides a specific service for their customers.
Speaker 2:Regardless of what fields you're in, the customer's needs is always primarily the entrepreneur's most focus and so there's such a need. And so, because there's such a need and because I'm seeing in my practice an overwhelming amount of anxiety and stress, the beginning of the year me and my associate are putting together stress anxiety 10 week module and it's a psycho educational group model to help with tools and techniques, empirical evidence tools and techniques that people can actually utilize on a day to day basis. It's such an overwhelming amount of anxiety and paralyzing stress that I'm seeing in my practice. We thought that these groups would be beneficial as a resource for clients for back and associates and local locals in the South Florida area to come to and sign up for. So we're putting that in place at the beginning of January. It's always assessing, it's always constantly do an evaluation of your business and the needs of your clientele.
Speaker 1:I love this. I was going to ask you if there's a lot of peer-to-peer groups. So the fact that you notice that there is this need and you've created this program for groups.
Speaker 2:We're experimenting it, we're doing it face-to-face and we're doing it virtually In the same week with Michelle Page. It's going to be leading my associates going to be leading the group. She's going to be facilitating because she knows the model, she's been educated on this model. We assess a need and we have a soft wait list happening. It's going to be a rotating thing, depending on the needs of the practice these groups and it's not a support group, it's not a dropping group, it's really supportive in nature but it's really about, like, leading the group with something to implement and execute in their day-to-day lives. That's really the key here. You have to have, like I said, a toolbox, and this group and these things that we're putting in place are toolboxes, tools in your toolbox, that kind of utilize so we stop out anxiety, we stop out stress, we diffuse it immediately. So we eliminate that from our whole core and our whole being by practice, by implementation, by experimentation, by execution, and do you counsel the spouses as well?
Speaker 2:Absolutely. The spouses are the ones that they don't get the focal point on them.
Speaker 1:Oh, absolutely, and they have. I believe it's called the secondary trauma. Secondary trauma yes, let's take a minute and let's talk about that real quick. Can we Sure sure, sure, yeah, yeah, let's do that.
Speaker 2:So secondary trauma is something different. It's being exposed to other people's trauma. So families, when their spouses come home and they talk about their day, that's a story they have to visualize. And that's again an example of secondary trauma. Hearing about being exposed to other people's trauma, a therapist, a story, a narrative about descriptions of things that are traumatizing for the first responder a secondary example of secondary trauma. These are all examples of secondary trauma and things that are passed down that can cause same symptoms of PTSD, same symptomology as PTSD, just by being exposed to secondary trauma.
Speaker 1:Absolutely, and then sometimes they feel like they don't have anywhere else to go to talk about it, you know.
Speaker 2:Exactly exactly, and that's why your social supports your informal. You have to have informal supports with your friends, your family, your neighbors, people that fill your cup, and you also have to have formal supports, professional people, professionals. You have to have an array of formal and informal supports that can help you professionally with intervention.
Speaker 1:Great advice. Do you have any final thoughts that you would like to share today?
Speaker 2:You know, I know this is being released around the holidays, but today is Veterans Day and I just you know my first responders, my veterans, my retired VA's, my nurses, people that help other people. They're the real heroes that they are trying their hardest, through the struggles and the trials and tribulations that they experience, not just professionally but personally, that they have to show up. They don't have a choice. They have to show up and they have to have compassion, whether or not they feel it or not. So those are the real heroes. The people that I help are the ones that give me hope and they give me. They fill me up professionally in reward. Just a mere fact of seeing the progress and seeing a first responder create levels of progression and benefit from the intervention brings me the reward.
Speaker 1:That's a great message of gratitude, especially for especially being Veterans Day. That is just a great message of gratitude. Thank you so much. Please tell us about your book.
Speaker 2:Okay, so the book right now currently is on my website, beckandassociatescom. It's under the shop tab. That version is only an e-book. It's coming on Amazon Kindle and Amazon Paperback. Hopefully by the end of November. We're going to try to push it out. So it's the compassion, the conundrum, first response strategies for first responders and service providers to prevent fatigue. It's really an educational tool for anybody who provides care Awesome.
Speaker 1:I look forward to that. So I'm going to get a copy. I just think it's invaluable information and it's something that should be shared, because many times we do not know what people are struggling with inside. Yes, and they might read something in there that touches them and gives them some direction and hope and encourages them to reach out. So again, thank you so much.
Speaker 2:You're welcome, thank you. Thank you for promoting it, because you know, obviously my goal is to help as many people as I possibly can, and so this is another avenue. Clientel is one, counseling is one, but also research, education, writing, publishing is another way just to educate and to bring awareness to the community and to people, people that are serving other people.
Speaker 1:Thank you so much, Michelle. Thank you for being my guest on the I Need Blue podcast.
Speaker 2:Thank you so much and for having me Again. It's always a pleasure to connect.
Speaker 1:You're so welcome, and this is Jennifer Lee. I am host of the I Need Blue podcast. You can find anything and everything you ever wanted to learn about I Need Blue on my website, wwwinadbluenet. And remember you are stronger than you think. Until next time.
