
The Cancer Pod: Integrative Medicine Talk
Join Tina and Leah, two naturopathic physicians with years of experience in natural medicine and cancer care. Leah is the ”cancer insider.“ Tina is the science-y one. Listen in and join us as we talk with each other or respected experts in integrative oncology. Whether it is you or a loved one, whether you are in treatment or beyond, you’ll find helpful info, tips, and tricks to get through tough times. We frame things around cancer, but honestly, anyone can benefit. So, tune in, join our community of like-minded folks, and please let us know what you think!
Disclaimer: This podcast is for education, entertainment, and informational purposes only. Do not apply any of this information without first speaking to your doctor. The views and opinions expressed on this podcast by the hosts and their guests are solely their own.
The Cancer Pod: Integrative Medicine Talk
Young Adults and Cancer: The Truth About Rising Rates and Prevention
The diagnosis of cancer is rising in young adults (under 45 years old). This episode of The Cancer Pod delves into potential reasons behind this trend, including epigenetics, environmental exposures, microbiome differences, and lifestyle factors. Tina and Leah discuss the types of cancers most commonly seen in younger adults, symptoms to watch for, and the significance of advocating for timely and accurate diagnoses. And, get ready for the next episode on cancer fakes and frauds!
Links we mention in this episode:
Cancer rates are 2-3 times higher today than two generations ago
Heavy metals (lead, cadmium, arsenic, etc.) in tattoos as a possible contributor
Why diagnosis of cancer is often delayed in young adults
Types of cancers more common in young adults
Young adults with colorectal cancer have better outcomes than older adults
The increasing rate of colorectal cancer in young adults worldwide
The SHIELD blood test for colorectal cancer
Become a member of The Cancer Pod Community! Gain access to live Q&As, exclusive content, and so much more! Join us today!
Check out our website! Looking for more information? We have blogs, merch, and all of our episodes listed by season and category.
Shop our favorite reads! We've joined with Bookshop.org to offer some of our fave books!
Have a comment or suggestion? Email us at thecancerpod@gmail.com
Follow us wherever you browse. We're always @TheCancerPod:
THANK YOU!!
Tina,
Tina:Leia.
Leah:it's kind of exciting. We have a membership now.
Tina:I would love to get to know some folks who are listening to us.
Leah:Yeah. So if somebody wants to join us in our membership in our cancer pod community, they can head over to our website and
Tina:Don't we become a pod of our own, like a pod of people?
Leah:we become a pod, which kind of makes me think of evasion of body snatchers, but, um, but anyway, um, yeah, head over to our website and you click on buy me a coffee, and if you want, you can just buy us a coffee, a one-time deal, or you can join our membership. We have three levels to choose from, and each one offers different bonus content and exclusive benefits.
Tina:We're gonna be doing live events with our membership so that you can ask questions. of course we cannot give medical advice'cause we are not your doctors, but we can give general advice
Leah:You can also, if you have any questions for us or comments, you can leave those messages on our website as well. The cancer pod.com.
Tina:and they can be good or bad. But if you have any critiques, then be constructive and help us out.
Leah:Don't be mean and remember to share this episode, your favorite episode or the whole podcast with friends, family.
Tina:We're really a resource now. I mean we have over a hundred episodes. A lot of them are very specific to side effects during treatment or challenges during survivorship after treatment. so It's becoming quite the library of information that if you go ahead and hit follow wherever you're listening to us right now, you can go back and find whatever you need in past episodes.'cause they are free and available.
Leah:And leave a review and rate us wherever you listen because that helps more people find us. And all of that helps us stay ad free, and that's important to us.
Tina:Yeah. And we can keep on doing what we're doing. Make it a podcast Since September, 2021.
Leah:so today we're gonna be talking about. It's been in the news about young people, younger people getting cancer. Um, are younger people getting more cancer? Are younger people getting cancers that are typically not common for people their age? So
Tina:Mm-hmm. And is this a phenomenon that is unique to the United States or is it more of a global issue? So we'll talk about that and more
Leah:stick around.
Tina (2):I'm Dr. Tina Kayser, and as Leia likes to say, I'm the science y one.
Leah:And I'm Dr. Leia Sherman, and I'm the cancer insider.
Tina (2):And we're two naturopathic doctors who practice integrative cancer care.
Leah:But we're not your doctors.
Tina (2):This is for education, entertainment, and informational purposes only.
Leah:Do not apply any of this information without first speaking to your doctor.
Tina (2):The views and opinions expressed on this podcast by the hosts and their guests are solely their own.
Leah:Welcome to the Cancer Pod. Hi Tina.
Tina:Hello Leah?
Leah:today we're talking about young adults and cancer,
Tina:Yes. Is the incidents on the rise and, uh, if so, why?
Leah:right? there are a lot of different theories out there. we have our own views yeah, so when they talk about younger people, it is typically people under, 45, I guess, is kind of what they're looking at. it's interesting because the study that I saw. Looked at two different groups. It looked at millennials and boomers, which is, you know, being a member of Gen X, feeling a little left out, especially because there are higher cancer incidence rates in Gen X as well. But they're looking at millennials and so that's people who are born between 1981 and 1996. however old that makes them. Dang it, my math is bad.
Tina:The youngest millennials will turn 30 in 2026.
Leah:Really?
Tina:Yes. You're getting old.
Leah:Oh my god. All right, so there are some cancers. I mean, I guess every cancer kind of has, its typical age range. And what's really unusual is that there are cancers that are more associated with older people. People over the age of 50, that younger people are getting things like pancreatic cancer, renal cancer.
Tina:You know, I just wanna put out there, this is not, I wanna say something right here at the beginning age. And the aging process is a risk factor for cancer. So you can't stop that one. There's only one way to stop aging, and that's not a good's not a good option,
Leah:It's not recommended.
Tina:right? So I'm saying that because right outta the gates, even when we say these are higher in younger people, it still is not near the rates of what people get after the age of say, 60, 65. We're talking about a different, it's higher in the age group, but it doesn't come close to what people are getting as they age.'cause aging itself is a risk factor that we can't do anything about other than not age anymore, which means that you're not here. So I'm saying that outta the gates.'cause I just wanna be very clear that even when we say the incidence is higher, it's still a very low incidence in a, in a global sense. Like when you're looking at the numbers compared to higher, ages.
Leah:And I think in, like in my work experience working at CTCA, I saw a lot of younger people who had breast cancer, colon cancer, you know, ovarian cancer, just more unusual, I don't wanna say unusual cancers, but I saw a lot of younger people because that's where people went.
Tina:Yes. Yes.
Leah:That's where they would travel to because of whatever care they were or were not getting where they came from because maybe they weren't diagnosed in a timely manner. Whatever happened then they would go to CTCA. When I went to Indiana the patient population was so much older and I think that is typical,
Tina:Mm-hmm.
Leah:for the most part. So anyways, that's just an aside. But yeah, so.
Tina:Can I say one more thing on a scale of aging? Even when we talk about young cancers, we're not talking about pediatric. So pediatric is under 18 years old, so that's a separate category and a separate discussion. We're really looking at young adults, which is, you know, like we said, really under 50. So round numbers is 20 to 50, and as you age within the 20 to 50 range, the risk does go up because aging is in there. That risk factor is still there, even. When you are considered a young adult with cancer. So that's all. I just wanna be very clear about the population we're talking about.
Leah:and I don't know where I saw it in my research for this, but, um, early onset breast cancer is considered younger than 45, and colorectal is considered younger than 50.
Tina:Mm-hmm.
Leah:And I do remember a long time ago, um, I. I was a big fan of the Today Show, and I used to watch, Katie Couric her husband was diagnosed with colon cancer and he was in his forties and that was really unusual at the time. he passed away and it was just, the whole thing was just really, I remember like, I wasn't working in, medicine, I was working in graphic design at the time, and I just remember just, it was just, it was all really surprising because it was so unusual. you know, now we hear about, I mean, not only people who follow us on. Our, social media, but you know, celebrities, um, Chadwick, Bozeman,
Tina:Hmm.
Leah:um, James VanDerBeek. You know, these are young people who, were diagnosed at a young age.
Tina:Yeah. And when we're talking about colorectal cancer, just like people over 50, people under 50 need to be screened. And if we can find that cancer at earlier stages, the outcomes are much, much better than finding it at a later stage of disease. in the grand scheme, bright sided to all of this, when you compare a people over 15, people under 50 with colorectal cancer, specifically, people who are younger do have better outcomes. They have less recurrence, they live longer. there's been studies that have compared, um, young adults with colorectal cancer from people who are over the age of 50. the outcomes are generally better. Now, I don't know if that's due to more aggressive treatment or just healthier because you're younger and you have more resilience built in. it doesn't matter. But on the bright side, um, it does have a better prognosis.
Leah:If it's diagnosed. And I mean, that's one good thing about the, the guidelines for colonoscopies being changed, and now it's 45,
Tina:Mm-hmm.
Leah:where it used to be 50 to get your colonoscopy unless you had a family history.
Tina:That was for Caucasians. It has been 45 for African Americans for a while.
Leah:Okay. but yeah, so if you had a family history, then it would be based on the age that, your relative was, diagnosed, But, am finding, and maybe this is just again, you know, because we have a certain population who follows us on social media, it's not always diagnosed in a timely manner when you are younger than 45 because it's being dismissed as you have IBS you have hemorrhoids,
Tina:Yes.
Leah:Al and I think it's the same with breast cancer. I mean, I don't know how many young patients I had who were diagnosed with breast cancer, under 30, who were told, oh, it's not breast cancer. You're too young to have cancer.
Tina:Honestly, that's where all those numbers that I'm talking about work against you as an individual. So you're an individual showing up at your doctor with whatever symptomology, x, y, Z symptoms. And that doctor is playing percentages in their head, like, what's the likelihood that this is benign? What's the likelihood that this is cancer? So they're gonna probably not diagnose it right out of the gates. So your, your age works against you in some ways in finding it early.
Leah:Yeah.
Tina:And I, I think that's a lot of the times the case. One bright spot there is for colorectal cancer, in July of 2024, the FDA approved a new test, a blood test for colorectal cancer that is just a blood draw. So in some ways it's easier to get. That done. and get your doctor to agree to just, can you just put that on my, on my lab or if you live in a state that allows it, you can order it yourself. depends what state you live in, in the nation.'cause healthcare in the United States is state by state. There are stool tests for colorectal cancer that can be done, but this is a blood test, so I feel like adoption will be faster than it was for stool testing, which is the Cologuard commercial with that little blue box that smiles and, yeah, it's the same company. This is called shield. The name of the test is, is called Shield.
Leah:Okay. And we could put a link to that in our show notes.
Tina:Yeah.
Leah:So, okay. So there are, five or six theories, as to why younger people are getting cancer or that they're being diagnosed with cancer. Um, and the first one is epigenetics,
Tina:Epigenetics?
Leah:which is different than genetics. So there is that, I guess we should start with that. So what is it like five to 10% of all people who are diagnosed with cancer? It's actually genetic.
Tina:Mm-hmm. I think we're gonna find out. It's depending on which type of cancer, I think it's gonna be when we finally find multi genes that put together, like if you have these three or five or 17 genes, do you have a high risk? We're getting there with that kind of data for single genes, like one gene, like the BRCA gene, BRCA mutation, or deletion So when it's a single gene, I would say it's gonna be 10% or so.
Leah:Okay, so we're not gonna talk about that. We're not gonna talk about the, the genetic component.
Tina:we did tackle genetic cancers once upon a time. It's in our catalog back in 2021 or 2022.
Leah:yeah. So again, we'll, we'll link to that. okay, so then the other word I said epigenetics. What, what are epigenetics, Tina?
Tina:Epi. Literally means above. So above the gene. So this is ways that our genes are turned on or off. So epigenetics has to do with regulation of the gene. And epigenes is very consequential. It is highly responsive to its environment. So for example, with epigenetics, you can unmask, meaning you begin to express a gene that's been silenced for generations and generations. But if your environment, literally your environment where the DNA is literally the cellular environment, what it's in needs, that gene it over time says, oh, we have reason to unmask this gene. Let's go ahead and do it. It will then uncover a gene that's been silenced. It's been sitting there, but it just hasn't done anything until you provoke it. And so we change our epigenetics more. Readily than the actual gene itself, which is made up of ATT c and g. You know that little spiral that we all think of A DNA looks like, right? It
Leah:All the way back to, to, you know, biology class.
Tina:Yeah. The helix, the double helix of DNA, that's a whole nother story, but the double helix of the DNA is att C and g and that does not change as readily. That's very difficult changing that the epigenetics is more fluid and changes generation to generation. So if my my great grandfather was a chimney sweep. that might have consequences on my epigenetics today because his body had to uncover genes to deal with the soot. Does that make sense?
Leah:Mm-hmm. Yeah. So your parents or grandparents' exposures, they have an influence on your epigenetics.
Tina:Yes, and it's generational, so it's very slow and hard to track. I think we are seeing some epigenetic results of what our grandparents and even our great grandparents saw when we had pesticides like DDT that were pervasive. Everybody was exposed to them.
Leah:Oh yeah, because we've, all heard stories about people running after the, the mosquito spring, the fogger, the truck that had the fog coming out the back. yeah, I remember like the planes going over, spraying pesticides, over certain areas in places where I've lived so.
Tina:Yeah. And the idea that the epigenetics is consequential, has been proven in animals again and again. So there's no, there's no dearth of information on this. There's plenty of information showing that, you know, it is not your parents, but your grandparents and even their, their parents that gets handed down. I think the most acute phase when this is happening is during pregnancy. I think that's a time that we have to really think about how things are being handed down because When someone's pregnant, when the ovaries in the fetus are forming, there could be consequences, right? Then that is when the genetics of that baby's children and whenever that baby goes on to have children. Those ovaries are already set. The stage is set for your ovaries in utero when you're a fetus. For men, it's different. Sperm comes and goes. Sperm generation is not set when you're a fetus. Sperm generation is now. And so I mean, that person should really be very, very, very conscious of no drugs, no alcohol, no, no chemicals, no pesticides, eat like super duper cleanly, all that kind of stuff.
Leah:They have to live in a bubble. They basically have to live in a bubble.
Tina:Well, you have to be conscientious, I think. I think that we can all. Do our best. It's impossible to be, you know, where we were before the industrial age. That's not gonna happen because even our air, in every city is, is not what it used to be. So,
Leah:Well, that can lead us to the another one, which is environmental exposures, right? So epigenetics and environmental exposures, they're very intertwined.
Tina:absolutely. Yeah.
Leah:And we have discussed this before. we talked about microplastics, we talked about forever, chemicals in different episodes. all of those. Play a part, yeah, I mean, once you become conscious of it, it's almost, I, it's, so for me it's very stress inducing because it's like every, there, there's just plastic everywhere. Everywhere.
Tina:I feel like when you start looking at clothing, you really start to go, oh.
Leah:right. With all the microfiber, the, um, sportswear, endurance, wear, hiking stuff, all of that. Yeah. We're, we're trying to shift more to products made from wool. but it's, it's hard. I mean, you look at your sneakers, you look at everything, you're hiking shoes, it's, it's just kind of everywhere. you look in your kitchen and it's just, it's shocking how much plastic, we have in our refrigerator and Yeah. In your grocery cart.
Tina:Yeah, I'm a fan of the old school, right? Like, just go backwards. You use glass, use ball, jars, glass is usually inert.
Leah:But when you buy something, when you buy, like things from a deli counter, you know, cheese or whatever, they'll ask, do you want us to wrap it in paper or plastic? And we're always like, paper. but not, not everyone has that. Um, so if you buy packaged cheese, it comes in plastic and then you go home, you take it outta the plastic and you put it in class. But it's already been, it's already been in plastic. It's, um, and I don't wanna go too much into this because we have talked about microplastics before.
Tina:Yeah. And they, they do disturb the gut.
Leah:Right? And they're found, I mean, they, they, they've been found in, throughout us, like in our, you know, our bodies. Um,
Tina:Even in the sacred space of the brain.
Leah:yeah, they've been found in the brain. They've been found in testicular tissue.
Tina:If they can pass the blood-brain barrier, yeah, they can go anywhere.
Leah:Yeah.
Tina:ultimately,
Leah:Yeah. And, but there are other environmental exposures too. you know, the forever chemicals are what we think of, like with the Teflon pan, when Teflon pan came out, those were just such a godsend. Everybody used Teflon pan and then they'd get scraped. And I remember'cause you're using the wrong utensils, and so then they get scraped and all that Teflon comes up. That is so bad for you.
Tina:Yeah. Yeah. And it's not so inert. I mean, if you're cooking over about 400 degrees, which is not difficult, then it starts to degrade whether it's scratched or not. So there are better alternatives now to that. it's really hard to track environmentally because we live in a soup, right, of so many different exposures. Our soil, our air quality, sometimes the water quality. So it's really a, it's not an easy one to track back and say, oh, you know, that exposure or that exposure. Every time we find one that's really focused upon like DDT or dioxin, we do our best to, you know, regulate that. But there is no, like you said, it's, a challenging one'cause there's nowhere that you can completely escape it.
Leah:No. And we have our, our cabin up in northern Wisconsin, and we have a septic tank. And when they come and empty that septic tank. Is everything that we use within the house and you know, the cleaners and everything that we put in there, everything is just very clean and natural. But I take medicine, I'm taking Tamoxifen, and so that is in that waste, and they will take that waste and they will spray it on fields. And the fields aren't necessarily growing food for humans, but it's out there. So, and you know, fortunately we don't take a ton of medications and so it's not, you know, this whole pharmaceutical soup that's in there, but like the thought that they're doing this from multiple homes and they're spraying fields and then the runoff will go into the river and the river goes, you know, down into wherever you know it just. That's crazy. Like, isn't that crazy that they're spraying human waste and what, like, that's not even the grossest part. Like, like it's everything that you put in there. And so they're finding, you know, they're, you know, p FFAs and stuff in there too. So, and then they're not P FFAs, P FFAs. Am I saying that right?
Tina:But you gotta tell folks what that means.
Leah:Well, those are forever chemicals. I'm not gonna break down what it, it's a
Tina:Well, yeah. Yeah. No, yeah. You don't have to say the word when you say P Fs, I don't. I think you lost people. That's
Leah:Oh, okay. Well, forever chemicals. Forever chemicals. And then of course, the thing that I brought up in previous episodes is I went to art school in the eighties and there was a lot of exposure to the solvents. Um, the coloring in oil paints that we would get on our hands, then clean it with solvents. We just like, we didn't care, you know? And so all of that.
Tina:Well, and I think a lot of folks still do that. Like they, they'll, I've seen it. People paint or they're doing work or they're like, I don't know. All sorts of people don't take the precautions'cause they think, oh, it's just gonna be, I do this all the time, or it doesn't hurt.
Leah:Right. Or I remember, um, like in photo lab, you know, we'd be in the dark room and we're just like pulling them out. You have little tongs, but you're just like, whatever. And you just grab it with your hand, you know, it's, you're 18-year-old thing and your photography professor is doing the same thing. So, so there're just like so many different ways that we are being exposed to things.
Tina:So back to the young adults with cancer, one of the things that we don't talk about, we we're talking about microplastics now, but there's also a lot of dyes in the, in these plastics, and there's been heavy metals used to make the plastics pretty colors. And so even in playgrounds, Playgrounds used arsenic in the wood. That wasn't good. They got that out and they started using plastics, and the plastics had, heavy metals in it. So there's, there's a lot of exposures that we've introduced because we don't have a system that makes sure something is safe. We have a system that double checks to see if it's toxic, and if so, at what amount? If we check it at all.
Leah:Even, um, tattoos
Tina:Mm. Mm-hmm.
Leah:and, you know, speaking as a tattooed person, you know, there are various heavy metals but depending on when you were. Tattooed. I don't know if they're making them healthier now. I have no idea. But, um, the tattoo ink, you know, different pigments that are used they have various heavy metals. and then that process itself, the inflammation that keeps your tattoo where it is
Tina:Yeah. And you know what's interesting about this? When we talk about heavy metals, you could argue those are natural. Because arsenic occurs in nature, as does lead
Leah:cadmium,
Tina:academy. They're all, these aren't synthetic chemicals we're talking about when we say this. So I just wanna say that.'cause you know, not everything natural is, uh, is okay in any dose either. So this is an example where it actually is not good,
Leah:Okay. So, We've talked about epigenetics, we talked about environmental exposures. There is also, our internal environment, our microbiome that also has been implicated in a possible cause for younger people getting cancer.
Tina:am very much into not just the microbiome of the gut, which we have a lot of information about. And we do have a lot of, indications that the bacteria that inhabit the colon. Or the breast ducts or the prostate. Those organisms when there's cancer are different than when someone does not have cancer. They have studies where they, they remove the colorectal cancer and then they look at the bacteria that are near the tumor. so the tumor has some bacterial populations that they name and then they look adjacent to it. same person, right? Same day, same surgery. The normal tissue next to the cancerous tissue has different bacteria in it. And so I think it's really young as a, as a discipline, like to figure out how the bacteria, and there's other organisms, there's viral particles, there's bacteriophages, which are a type of virus. There's yeast in other fungus. So there's a, there's a whole community ecology everywhere that there's bacteria, uh, that we say bacteria because it's the dominant population and there's more of that than anything else. But the others may not be minor players. They could be big players in some of the cancers. We don't know. So I, I think I'm way into the microbiome, not just with gut, but of the actual cancer. I'm trying to get the word onco biome to, to take hold. You know, if you look for onco biome right now, you're not gonna see much. But I think it's the apt term for when the bacterial communities are actually inside the tumor. They're in the cancer, which is heresy 20 years ago. That's like, nah. All inner organs with the body are sterile. They're not, we now know that there are actual bacteria inside certainly inside the tumors. And so not only are they there at the primary tumor, but they're there when you look at the metastasis of a tumor too. So a colorectal cancer, you can look at the tumor, look inside it, you'll see certain bacteria. There's one called Fusobacterium, nucleotum that's really implicated. Um, totally normal to have that in your mouth. You're not supposed to have it in your colon. So it's like, I always think of like ivy or Kudzu, you know, like it's totally normal plants somewhere else. That's what I think of with these bacteria and cancers like that Fuso. Bacterium. Nucleo is totally normal in your saliva and no problem there, but when you find it in the gut, it in, especially in the colon, it is associated with colorectal cancers and it's actually inside the colorectal cancer. And if that colorectal cancer happens to go somewhere else in the body like the liver, and you take that tumor outta the liver, it's inside the tumor that's in the liver. So I mean, this is like, I'm trying to get onco biome to like really catch on and I'm like, that's what it is. It's an onco biome oncology cancer biome. Like it's a specific to that cancer. But we'll see. We'll see if it evolves. There's a few papers that use the term, but it's not commonplace yet. I encourage all of our listeners to go talk about onco biomes.
Leah:well, what I, what I thought was interesting is I found, um, something that talked about how the biodiversity of the gut in younger colorectal cancer patients is different than the diversity of the microbiome in older patients with colorectal cancer. I thought that was really interesting too.
Tina:You mean it's less diverse or
Leah:they had less diversity than with an older patient.
Tina:Okay.
Leah:so that's like another thing where it is not necessarily the same environment, and so what some of the things that might be altering a microbiome, the medications that we take, antibiotics,
Tina:Antibiotics are independently linked to higher risks of cancer. Various cancers, breast cancers, colorectal cancers. There's many cancers that are associated with higher antibiotic use in the past.
Leah:And so what, what would higher use be? Is there a definition for what's higher use?
Tina:No, it's a, it's a dose, linked association though. The higher your antibiotic use in the past, it associates with a higher rate of incident cancer later.
Leah:And so that would, that would have to do with your diversity of what's living in your, in your gut.
Tina:Absolutely. Maybe we did use antibiotics more in certain decades than others.'cause we, we backed off, but only more recently
Leah:No, that's true. Yeah.
Tina:they're being used a little bit less. But man, I think they were, antibiotics were given out like candy in the, in the eighties. Nineties,
Leah:Well in, in seventies, I mean, in our, you know, more our kind of growing up generation, um, whether or not you were a C-section baby that definitely plays a part in your microbiome.
Tina:yes.'cause you get your organisms from the vaginal canal.
Leah:Yeah. Um, breastfeeding. Were you breastfed? Were you bottle fed? And so all of these, you know, there are trends, right? I mean, when I was a baby, I think I was breastfed for a few months and, you know, that, that whole formula thing, like when I guess formula came out, it was a godsend, right? I mean, it just kind of. Save time. Women could work You know, like if their babies were fed formula, they could go back to work. and then it started to trend back to breastfeeding. So it, yeah, it is interesting to see like that, you know, even with, with having a c-section, you know, you have one child as a C-section and then all your children are C-section. I don't believe that's how it is anymore. your diet, I mean, that's kind of like the most obvious thing, right? Like your diet. How does that affect your microbiome? It's everything.
Tina:it's everything. Generally speaking, diversity in the gut. If we're just talking about what's going on in the GI tract, diversity is your friend. so you do want diversity means that there's a lot of different types of organism. There's a lot of variety in there. So diversity is your friend, diversity in your gut, which comes from diversity in your diet of plant foods.
Leah:Yeah.
Tina:Yes. So that's, that's if, yeah, if, if you wanna know what to do, you eat more color, it always comes back down to the same thing, same advice. Eat a lot of plants and a lot of different types and a lot of different colors. Leaves and stems and flowers and roots and tubers and, you know, mix it all up and you'll eventually, um, have a very diverse and healthy gut.
Leah:And we've talked about before, having that 30 different plants in your diet a week. So that includes the spices, the herbs, you know, your grains, all of that legumes. I like saying legumes.
Tina:Yeah. You know, and probably the easiest way to do that is you have a little chart that you can, that's almost like a little laminated thing. They, they sell these, usually it's for kids.'cause we're we're trying to get kids to eat better. and just make sure that that day they had something yellow, something red, something in the blue spectrum could be blackberries that counts. Accounts purple. So just make sure that there's lots of color. And if you do that, you know, every day, all the colors, you'll probably get enough variety. Doritos don't count. I always have to add that.'cause that's the first thing people ask me is like, Doritos. And
Leah:Oh, you're kidding. Oh, that's funny.
Tina:Yeah. Well,'cause I think like Cheetos and Doritos leave all that orange stuff on your hand, so it's the first thing people think
Leah:that's not, I mean, and they are plant-based, so I guess I could see their argument there. But, um, yeah, and, and again, even the brown foods, right, the grains, the beans.
Tina:Mm-hmm.
Leah:Don't dismiss those either. It doesn't just have to be what's in the rainbow. It could be just what's in the full spectrum. Look, the Crayola box. Let's start, let's start that. Eat the,
Tina:Eat the Crayola. But is it the 16 count or
Leah:No, it's the same. I'm going for the 64. The big box with, with the big box. With
Tina:Well, I, I'm thinking daily. You're thinking weekly.
Leah:I'm thinking we, yeah, I'm, I'm going. But that, in that case it would be the 32. Anyways, uh, we're, we're digressing. okay. And so then speaking of, of diet influencing the microbiome diet in itself, the highly processed
Tina:Calorically. Dense.
Leah:ultrapro, calorically, dense, nutritionally lacking devoid, that's a good word. Um, foods, uh, sedentary lifestyle. obesity. Obesity is a risk factor.
Tina:Yeah, so, so each of those are independent risk factors. And when we say that, that means that there are plenty of studies to show that ultra processed food is associated with higher risk. And I do think we have introduced those multi-generational now, right? So we have people who grew up on highly processed food and then went on to have children on highly processed food. So I think some of those epigenetic effects are due to. Some of the multi-generational now changes in our diet, in our, in our lifestyle. So yes, the calorically dense foods that lead to obesity in our sedentary lifestyle,
Leah:Sedentary lifestyle. I mean, we had PE in school, you know, are kids still going out and playing pe? I don't have kids. I don't know. But it seems like a lot of things are getting cut in our schools
Tina:know, that's a really good point because if we say highly processed food is associated with cancer, exercise is associated with less cancer. So another way to frame all of this is exactly that. What if we stopped doing that was. Anti-cancer, like maybe what we should be looking at is not what causes it, but what was preventing it in the first place and making sure that we add those back, which is a little bit more empowering than just saying, you know, what causes it.
Leah:And again, there may still be PE in schools. I just remember it was like an hour of, playing soccer or softball or volleyball or whatever.
Tina:So let's be honest, there was that hour and then there was all sorts of other hours because we didn't come home and jump on a game box. We came home and went and did stuff.
Leah:That's true. Yeah.
Tina:We didn't, we didn't sit around. We literally didn't just sit down'cause we were kids and we had a lot of energy. And so, and I'm thinking just in, even in school, it would be like I had a free period and you know, we'd ask the gym teacher, can we borrow the cross country skis and try to, you know, go down the hill over there. And she's like, okay, sure. So we did all sorts of things.
Leah:Okay. You went to a completely different school than We never had cross country skiing in any of the schools I was at, but, um, that's, that sounds kind of fun actually. but yeah, I was in drama and so we were dancing, you know, we were doing all of that sort of thing. But yeah, we weren't sitting around in front of a, a monitor playing games. I did watch a lot of tv, but yeah. But I would also go in the backyard and, you know, try to practice softball'cause I was horrible at it. Or climb trees, all of that stuff. We were outside more. It doesn't explain why our generation also is getting,
Tina:Well, we were outside more, but we also were not being monitored, so maybe we were like literally like the classic, be home by dark. And so it's, I don't know about you, but I went all the way down to the park in the village, across the golf course, down the hill. I'm like,
Leah:oh, we were riding our bikes. Like
Tina:yeah, at very young ages we were out and about going, traveling around is my point. So that,
Leah:we sound like old people. We sound like old people right now. Being like, back in my day I used to walk uphill both ways to school. yeah. But definitely it's, it does seem, it, I mean even my, like now I feel like I'm more sedentary with social media. Like I'm way more sedentary than I used to be.
Tina:Oh yeah, me too.
Leah:Like it's,
Tina:this, these screens that were staring at a lot of my work is on a screen. Yeah.
Leah:Yeah.
Tina:Admittedly, I'm not out and about. Going to the park?
Leah:no, but I am currently in Tucson and it is lovely weather here, and I have been walking the dog for about half an hour a day, which isn't a terrible long time to walk, but I wear a weighted vest even to kinda up my game. So there's 30 minutes of my 150 minutes. A week
Tina:right?
Leah:my exercise. And so I have been doing that. I've been here, I don't know how many days, but yeah, I mean it's a good habit to get into moving. moving. Even if, and this is something I would tell my patients all the time, just put on some music. Put on a song, and dance to it. Everyone's got a song. You don't like dancing, just move to it. Move.
Tina:I like it.
Leah:so, anyways, okay. So yeah, so, another thing that I have read is a theory as to why there may be you know, more diagnoses of cancer in young people. sleep.'cause we were talking about devices, um, being on social media, all of that causes alterations to our sleep cycle. And so sleep is when our body repairs. If you're not getting a. That repairing going on, that is bad. That's really bad.
Tina:Yes. I think if people do wanna pursue that as. Where the evidence is light at night, LAN has been studied extensively and light at night is associated with higher cancer incidents. we have a lot of light at night now. I mean, all you have to do is look at a map and see how bright cities are. You can see it from satellite images. there's something called clock genes that's probably at the heart of this. So we should respect the circadian rhythm that we associate with our best health and our best function. That is you sleep at night and you're awake in the day, you eat in the daytime, you don't eat in the night. You know, there's these little cues, biological cues that you send your body, that help it normalize its function, whether it's immune function or endocrine function. and certainly brain function is best when you. Get a good deep sleep, you get these waves of glymphatic that clear the brain. And so there's no downside to this is my point. And if you don't, if you do have light at night when you're sleeping, put something on, put a mask on, um,
Leah:Eye mask,
Tina:yeah. Put a eye
Leah:a sleep eye
Tina:Mm-hmm. Yeah. If you can't make it pitch dark, then, then that's your second way of doing it. And a lot of folks like to do that because then you can pick the mask up if you have to go to the bathroom and see where you're going.
Leah:The other thing you can do is, because there are devices, like we have a HEPA filter in our room and I put tape over the little light'cause there's like a dim function where you can kind of dim the light of the HEPA filter, but there's still a little light. And so you could just put like several layers of, you know, tape over that light.
Tina:Yes. Very important. It's essential. This is like foundational, this is like eating your veggies, get, get a good night's sleep. And total darkness is really important. the last thing we wanted to talk about was early detection, right? I mentioned it a little bit early in the show, but detecting things earlier is always a good idea.
Leah:Well it And is that, why is early detection, why, you know, because imaging is getting so much better. Is that why more cancers are being found?
Tina:Mm,
Leah:are, is it just because like imaging is so much better?
Tina:I don't think so because most of the colorectal cancer is stage three and four. That would've been picked up on, um, CAT scan of 20 years ago still would've picked it up. Oh, I do wanna say this though. I don't think this is connected to Covid at all. Like I should say, we can't blame the Covid pandemic in any way because a lot of this has happening in prior to 2020.
Leah:Right. So there were, uh, there were the conspiracy theories that it was not only Covid, but it was also the Covid vaccine. this trend of younger people being diagnosed with cancer started in the nineties.
Tina:Yeah. Yeah. And it's just gone up since. I will say this though, whether it is infection or a vaccine, anything that causes systemic inflammation to be kicked up can cause cancer to grow faster at that time, progress faster. So systemic inflammation, whenever there's a tumor, systemic inflammation generally means that it's going to grow, it's gonna cause it to grow. We've done this in animals repeatedly'cause we have an experimental model with animals where the poor little things we, we create inflammation in their little paw pads and then we see what happens in other parts of their body. So. We've done this multiple times with, in multiple experiments with animals, and I don't think it's any different for humans. Systemic inflammation can cause a cancer to grow.
Leah:It could be caused by, Infections that aren't being addressed. Um, different exposures there was an article from University of Chicago and they were talking about chronic inflammation as being a potential reason.
Tina:Yeah. Chronic inflammation is a potential reason, and you still need the microbiome in that area to be. Skew. there was a model, it was actually done in the journal science. It was a model where they used h pylori and they, they proved that h pylori was connected to stomach cancer, but only under certain conditions, and it had to be chronic inflammatory conditions.
Leah:And that is one of the cancers that, um, we are seeing more and more young people getting gastric cancer.
Tina:Yeah, and I, I'm sure that's a delay of diagnosis because generally speaking, that's not gonna be suspect in people who are young. it's not as common as breast and prostate and colorectal cancers and other cancers like that. So it's gonna be way, way down on a doctor's differential diagnosis. So yeah, I could see how that's a delay of diagnosis a lot of the time too.
Leah:another possible theory was, people were giving birth later, they were having fewer children, and also, waiting to have children and that would lead to a higher risk of breast cancer and potentially ovarian and uterine cancer.
Tina:Interesting. Sure. Yeah. having children lowers your risk.
Leah:And I think. A really big one, um, that we see in the United States healthcare disparities, so people not having access to, medicine, to doctors, to healthy food. That in itself is a risk factor for cancer at any age, but, um, definitely can affect younger people.
Tina:I I think that most people probably don't get taken very seriously when they go in. If you're under 45 and you have symptoms, they're gonna think it's other things so, so the other piece of advice is be persistent. If you do see the doctor and they don't help you go back and tell them That didn't work. What else you got? So I think it's really important to not, stop until you're symptom free is really basically it. And that should be not stop until you have a good diagnosis.'cause even without symptoms. You can, you can allay a symptom but still have the problem underlying it. You know, you could take a drug and stop, uh, I don't know. You could stop diarrhea. And, and well that's not really helping if you don't have a proper diagnosis. So always make sure you know the condition that's causing it. And if you're not getting that persist, it's not always easy to advocate, self-advocate, but, you know, bring someone who likes to do that kind of stuff. There's, we all have those people in our lives. I am one of those people, so I know.
Leah:Okay. So we've been talking mostly about like breast and colorectal. We mentioned gastric cancer. So what are the cancers that we are seeing higher incidence in younger patients?
Tina:Mm-hmm. At, at least in the us. Um, according to the American Cancer Society, the most common cancers in young adults are breast cancer lymphomas, both non-Hodgkin and Hodgkin melanoma sarcomas. cancers of the female genital tract. So that's cervical and ovarian cancers, thyroid cancer, testicular cancer, colorectal cancer brain and spinal cord tumors. So those are the most common, according to the American Cancer Society here. doesn't mean they're all increasing in incidences. We have talked about a couple that are, but those are the ones to look out for
Leah:Yeah, and I had read that, those cancers, so colorectal, breast, prostate, uterine, gastric, small intestine. Kidney and pancreatic cancers are three times higher in patients born in 1990 versus 1955.
Tina:oh, wow. Three times higher. That's, that's a lot. Yeah. Well, and I just wanna say the other thing, which is, you know, maybe people are curious, like, how do I know my symptoms, even a symptom of cancer? And I'm gonna go through the quick list by the American Cancer Society for that too. an unusual lump or swelling, especially in the neck, breast, belly or testicle. So get that checked out if you feel something. Unexplained. Tiredness and loss of energy. And that's usually profound, right? Easy bruising, abnormal bleeding, pain in one part of the body that just won't go away. Unexplained fever that won't go away. Frequent headaches sometimes if that headache comes along with vomiting, obviously not if you have a cold or a flu, but if it happens repeatedly, I would put on here night sweats. So middle of the night you get all hot and sweaty. that's my own addition. Sudden eye or visual changes, loss of appetite or unplanned weight loss. Don't explain it away. If you have unplanned weight loss, you do need to get that checked out. And then of course, for your skin, a new mole or other spot on the skin or one that changes. Shape, color, or size. That's all the signs or symptoms.
Leah:And then some considerations for younger adults when they are diagnosed with cancer. talking to your doctor about, fertility preservation is really important. treatments can cause sterility so whether, so whether that's, you know, like a sperm bank or cryo-preservation, where you're retrieving eggs and saving those, you know, those are really important conversations to have. and I think that's frequently missed. and then how do you talk to your kids after you've been diagnosed? Finding someone, finding resources to help you talk with your children after a cancer diagnosis. you can talk with your care team and see if they have resources for you, and then talking to people about, you know, the, the impact on, on your work. You know, do you talk to your employers? how do you like juggle going through treatment and working,
Tina:Most can. Centers do have, counselors and social workers, and I think they're underutilized. I think you shouldn't wait for a referral. You need to advocate for that too. I think it's really helpful. I think it's something that we as professionals should also make more use of. I mean, it came to the point where I felt like everyone should do an interview with, with the team, whoever the counselors and social workers are at a given center. I know they don't, they're not usually staffed to the point where everyone can go see them, but boy, would that be awesome because then people don't have a, I don't know, what's the word I'm looking for? preconceived notion as to why they're being referred there. Right? Like, you know, I think PE it's hard for us to admit we need help sometimes and especially emotionally. So I think it'd be great if it was everybody got screened.
Leah:I mean, both cancer centers I've worked at, they had patients during intake process, meeting with counselors and.
Tina:Yes, making it universal removes the taboo.
Leah:Yeah, for sure. I know one of the big concerns that I have seen on social media, and read in articles, the concerns about how do you date with cancer, with a cancer diagnosis, and talking about sex with an after cancer. these are big topics that, find someone to talk about that with, like, reach out, ask your oncologist, ask your team.
Tina:Because there's physical and psychological barriers or hurdles often after cancer treatment.
Leah:Absolutely. Okay. So, um, if you are listening and you are a. A person who has not been diagnosed with cancer and does not have a history of cancer, what are things you can do to reduce your risk? We've mentioned some of them so far. Trying to improve your sleep, your sleep, environment. adding diversity of plants to your diet. reducing ultra processed food, reducing processed meats, and reducing alcohol. These are things that we have talked about. Oh, increasing fiber. That's another one. So that's part of your plant foods. Right? You're increasing fiber. You're increasing those, those colors I think we've covered all of these.
Tina:I know I was thinking the same thing. We've actually discussed each of these at length.
Leah:Yeah. As I'm going through the list, I'm like, wait, that was this episode? That was that episode. I think. Did we talk about processed beets? I don't know, but I'm sure we've mentioned them before.
Tina:yeah. And I mentioned how sleep is so foundational. We actually had two episodes on people who have trouble sleeping. So if people go back to that, we're very specific on what you can do, conventionally and with, with natural agents to help with sleep and,'cause there's different reasons that we, you know, wake up in the night or can't get to sleep in the first place or whatever. So we have addressed that. You're right. And then we've addressed alcohol. Yeah.
Leah:we've addressed fiber. We just talked about ultra processed foods. So Yeah, actual items. We got all, we got all the resources for you.
Tina:The ultra processed foods is in the, seed oil episode. So that's just our last episode before this one.
Leah:Yeah. And we're both kind of excited about our next episode. Oh my gosh. Well, I really enjoy it because part of our assignment for research is watching Netflix and Hulu, which is one of my favorite things to do,
Tina:So I wanna ask our listeners to do this too, where ask people to go ahead and watch some of these programs so that the follow up podcast will make sense,
Leah:yeah. So we are talking about, fakes and frauds people who lied about having cancer. so we are watching Anatomy of Lies.
Tina:which is, I gotta say this, which is about a writer who wrote for Grey's Anatomy and she was a faker of cancer.
Leah:oh, she was a faker of so many things that, that is. So,
Tina:Diabolical
Leah:oh, it's just insane. It's insane. Um, and then why don't I remember the other things we watched?
Tina:Scamanda.
Leah:Oh, Scamanda, that's on Hulu.
Tina:Yeah. That one feels a little bit like a Hallmark movie, but you know, it's still worth watching.
Leah:the thing with Scamanda is it's a b, C news and so it's very much like if you were watching like Nightline or or one of those a b bbc Well, they, they like kind of, they, they repeat a lot of stuff.
Tina:It's the one you can kind of be watching while you're doing something else'cause they repeat themselves.
Leah:Yeah, I was doing a lot of rewinding it. It's really interesting. Um, and then the third one is we're gonna, to, we're gonna talk about Bell Gibson. And so,
Tina:Not Mel Gibson, bell Gibson.
Leah:Mel Gibson's a completely different episode, but yes, we are talking about Belle Gibson and I'm sure many of you have heard of her. she was in Australia and she. Pretended to have cancer and really created a huge following. Well, we'll go, we'll go into it more in, our next episode. So that's what we're recording next. And so right now we're just doing the research by watching these.
Tina:We're doing the research. This is hard work folks.
Leah:It's my favorite kind of research. Okay, so, um, again, thanks for listening. And
Tina:That's a, that's a loose use of the term, but go ahead.
Leah:again, if you like this episode, leave us a comment, leave us a review, a rating,
Tina:Yeah, give us a shout out. Email us, you know, we're around.
Leah:share the episode with your, with your friends and family.
Tina:And consider us a resource when you need us.
Leah:On that note, I'm Dr. Leah Sherman,
Tina:And I'm Dr. Tina Kaczor.
Leah:and this is the Cancer Pod.
Tina:Until next time.
Podcasts we love
Check out these other fine podcasts recommended by us, not an algorithm.

Natural Medicine Journal Podcast
Natural Medicine Journal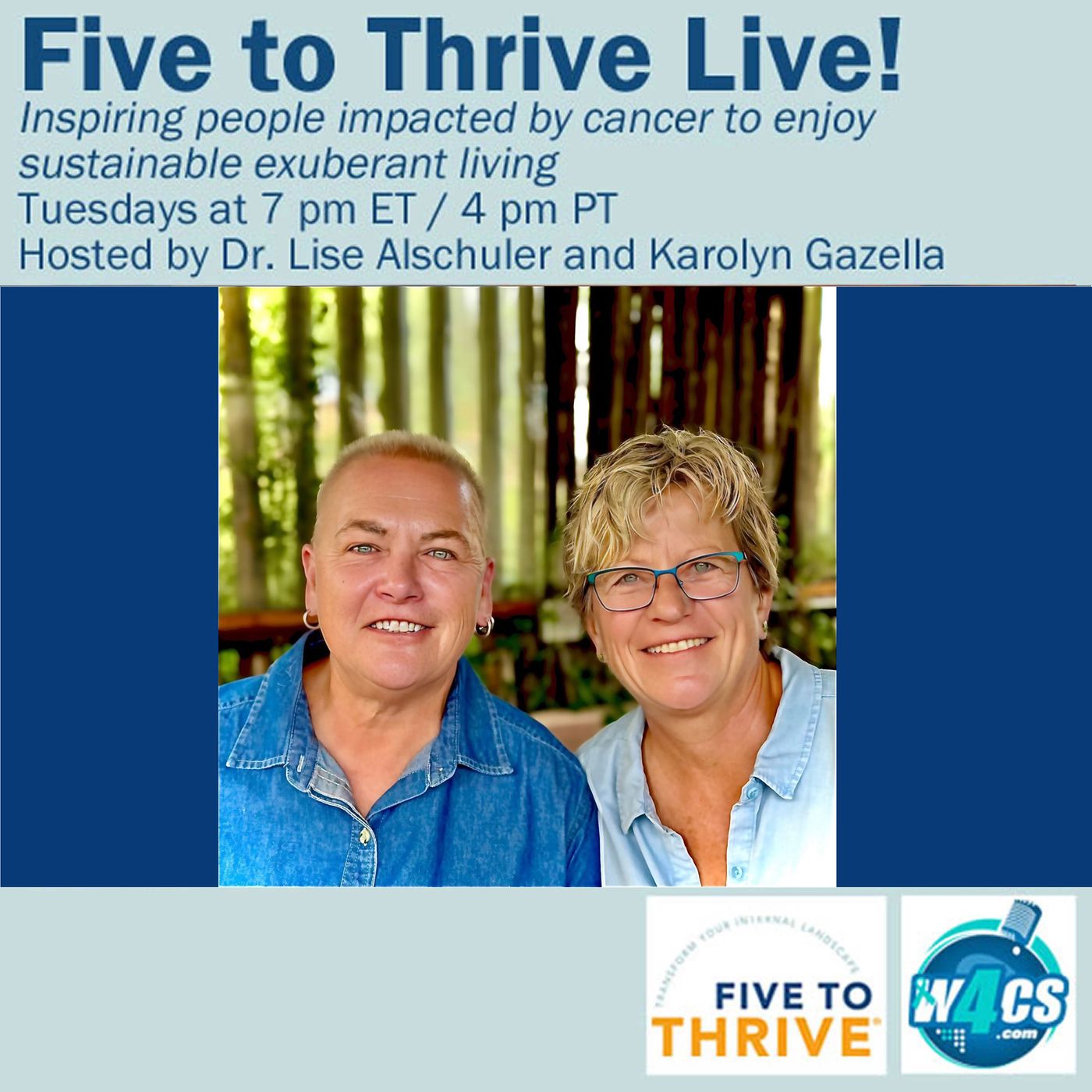
Five To Thrive Live
Talk 4 Radio
Huberman Lab
Scicomm Media