The Conversing Nurse podcast
Are you a nurse curious about the experiences of other nurses? For 36 years, I have only known the Peds/NICU realm but I am intrigued by the roles of nurse researchers, educators, and entrepreneurs. Through conversations with nurses from various specialties, I aim to bring you valuable insights into their lives. At the end of each episode we play the five-minute snippet, just five minutes of fun as we peek into the 'off-duty' lives of my guests! Listen as we explore the nursing profession, one conversation at a time.
The Conversing Nurse podcast
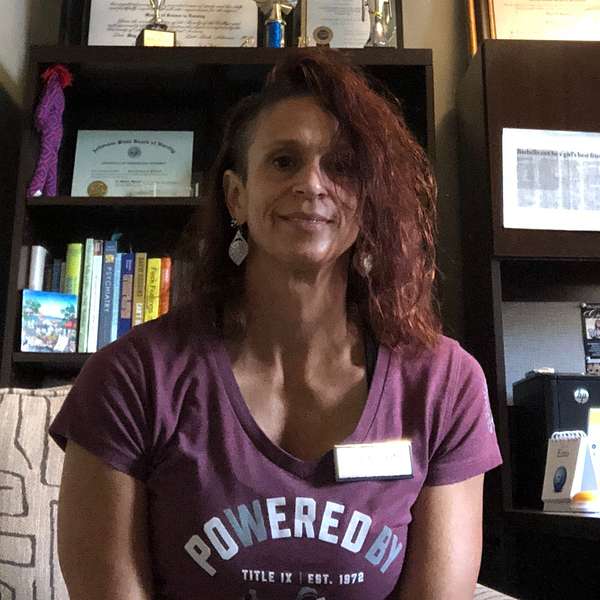
PMHNP and Powerlifter, Tara Kittrell
**CAUTION** In this episode we discuss mental health, including suicide. If you are experiencing mental health challenges and have thought of harming yourself, there is help for you. Call or text 988, the Suicide/Crisis Hotline. Help is available 24/7/365. Please reach out.
What do psych nursing, powerlifting, and The Walking Dead have in common? My guest for this week, Tara "Taz" Kittrell. Her long career serving the mental health needs of women and children has progressed from a foster care case worker to a counselor, then as a sexual assault nurse examiner to a pediatric post-op nurse, to what she does today, serving college students as a psychiatric mental health nurse practitioner. Now, I could stop here, but I won't because there is so much more to her story. Tara is currently enrolled in an EMT Basic program, and when I asked her why, her answer just lifted her higher on the pedestal I had put her on. And did I mention she happens to competitively deadlift? When Tara wants to get out of her head, she gets into the gym. Her powerlifting efforts have won her several prestigious awards. She strongly believes in the power of movement to improve mental health, and she shares this love with her colleagues and students. In the five-minute snippet, there are 27 callers ahead of you. For Tara's bio, visit my website (link below).
Tara's Instagram
Tara's LinkedIn
Lifting Heavy Things- Healing Trauma One Rep at a Time by Laura Khoudari
Built to Move-The Ten Essential Habits to Help you Move Freely and Live Fully by Kelly Starrett
Contact The Conversing Nurse podcast
Instagram: https://www.instagram.com/theconversingnursepodcast/
Website: https://theconversingnursepodcast.com
Your review is so important to this Indie podcaster! You can leave one here! https://theconversingnursepodcast.com/leave-me-a-review
Would you like to be a guest on my podcast? Pitch me! https://theconversingnursepodcast.com/intake-form
Check out my guests' book recommendations! https://bookshop.org/shop/theconversingnursepodcast
I've partnered with RNegade.pro! You can earn CE's just by listening to my podcast episodes! Check out my CE library here: https://rnegade.thinkific.com/collections/conversing-nurse-podcast
Thanks for listening!
[00:00] Michelle: What do psych nursing, power lifting, and the Walking Dead have in common? My guest for this week, Tara Taz Cattrell. Her long career serving the mental health needs of women and children has progressed from a foster care case worker to a counselor, then as a sexual assault nurse examiner to a pediatric postdoc nurse, to what she does today serving college students as a psychiatric mental health nurse practitioner. Now, I could stop here, but I won't because there is so much more to her story. Tara is currently enrolled in an EMT basic program, and when I asked her why, her answer just lifted her higher on the pedestal I had put her on. And did I mention she just happens to competitively deadlift? When Tara wants to get out of her head, she gets into the gym. Her powerlifting efforts have won her several prestigious awards. She strongly believes in the power of movement to improve mental health, and she shares this love with her colleagues and students. In the five-minute snippet, there are 27 callers ahead of you. Well, good morning, Tara. Welcome to the podcast.
[01:38] Tara: Thank you so much, Michelle, for having me because I've been listening to your podcast and it has been a wealth of knowledge hearing about other nurses in other disciplines. I love it because when you get stuck, or I don't want to say stuck, but in your field, you sometimes forget there's other fields out there. And it's just fascinating to hear other people's perspectives, even when you interviewed somebody in my field. So thank you for your podcast.
[02:09] Michelle: Well, thank you, Tara. I appreciate that. That's why I do it because I don't want to say I was stuck in the NICU for Peds and NICU for 36 years but we didn't get out much.
[02:26] Tara: Right.
[02:27] Michelle: We didn't really know that. There's this huge world of nursing. I just am excited to, and I consider it an honor to have spoken to so many great nurses in all these wonderful fields and your field as a psychiatric mental health nurse practitioner until I interviewed Kirby Williams last year. I was so embarrassed, I had never heard of that specialty before and it's fascinating. So we'll talk a lot about that today and we'll just talk a lot about everything because you have a very full bio and you've done a lot. And we'll talk about your athleticism or that you are an athlete, because one of the things that really jumped out at me when I learned about you was your Instagram. So it's @Tarathewalkingdeadlifter. And it really grabbed me because of two things. First of all, The Walking Dead.
[03:33] Tara: Yes.
[03:34] Michelle: I didn't know if that was it. Love that series.
[03:40] Tara: It was my favorite show. And then there was Tara. And I love it, was just, it was perfect.
[03:49] Michelle: That is perfect. And then the deadlift, because I will classify myself as a former crossfitter. I did CrossFit for two years, and then the pandemic hit and it just all went to shit. So we'll talk about that because I'm very sure.
[04:04] Tara: Yeah.
[04:06] Michelle: So one of the things in your bio is I noticed a thread, you have a long history of working in the mental health space, particularly with women and children. So I'd love to hear more about that.
[04:24] Tara: I guess I should start where initially, I went to school to be an athletic trainer, and I was a student athletic trainer in high school. Then I started college to do it. And I loved the women's gymnastics. I was put on men's gymnastics. Love that. Then I was put on football, and I hated it. And it was before we appreciated concussions, CTE, and all that. And I would be tasked with telling football players, you can't play. We're all from the Northeast, and you getting cursed at and then you curse them. It wasn't a good fit. So I then was like, well, what do I do with myself? I didn't want to spend a lot of time in college, so I had enough credits to finish as a health education major. But I was offered a teaching position where I student-taught. And also, I was a former. No, not a good one. I was really good in high school. But then when I went to college, I was fair. Maybe I could get a point or two for the team. But I was a collegiate runner my freshman year. But I've always been drawn to athletics because I grew up playing, know all that. So I was kind of like, well, what do I do with it? I went. I was on a bus going home. I went to college in Springfield, Massachusetts, and I grew up right outside Boston. And I was on a Peter Pan bus because that's what we had. And I was sitting next to a woman who turned out, she just opened up, told me her life story. She was a prostitute. And I was listening to her. She was telling me all the drama about being out on the streets and blah, blah, blah. And she asked me, what are you studying? And I had a psychology book, taking it basically just as a core requirement, but I wasn't even a psych major. And she said, you're really good at listening to people. And I started thinking, and she says, you don't judge me. You're good at listening. Now, I talk a lot, but I also listen. And so we're having a dialogue. And then obviously I'm a woman and all that. I shouldn't say obviously, I'm sorry, but I identify as a woman, a cis woman, and it just always been drawn, obviously, to working with women and children. And I think from that, that's what kind of set it off. And then I went into a counseling program, went to the University of Georgia, and I got my master's in before, and this was, I guess, where the fork in the road was. I seriously thought of going to Tutulane University to study public health, but with a specialty in maternal and childbirth because of just, you probably could speak better to me just about all of the issues with birth and just we as a society, how we don't take great care, and there's so much systemic racism. And more importantly, even though we're a developed country, our infant mortality is really disturbing.
[07:23] Michelle: So true.
[07:24] Tara: Yeah. So sorry for that whole thing, but that's kind of what led me to it. And then it just seemed I had just kind of the jobs, they just kind of branched and evolved.
[07:37] Michelle: I love hearing the stories. I've said many times during my episodes of talking to nurses about asking why they got into nursing or what attracted them or how did it happen. And so many times it was just kind of like a fluke. It was just something that they never had really set their goals on. But somebody recognized something in them that spurred them in that direction. And that's fascinating.
[08:12] Tara: And, Michelle, here's the wild. You know, you interviewed, you know, D. D. Finder and I are siblings. We're both a, we were not groomed to be nurses, which is strange. Our grandmother was a nurse. Our mother is a nurse. We have two aunts who are nurses. We have a cousin who's a nurse. And I always, strangely enough, thought I wasn't smart enough to be a nurse. I just thought I wasn't smart enough. But then I ended up going to nursing school at 30. I don't mean to be that person, but I graduated with nursing honors, so apparently I could handle the work. But I just think just my experiences and how I was raised and I struggled when I was younger in school, in certain subjects. I just thought I wasn't smart enough to be a nurse.
[08:59] Michelle: That's so interesting. D. D. had told me the same know a lot of nurses in the family and the same large Catholic family.
[09:10] Tara: Yes.
[09:11] Michelle: Eight kids and six are nurses.
[09:14] Tara: Wow.
[09:15] Michelle: Yeah, it's pretty crazy, you know, this growing up at holidays and lots of people at Thanksgiving, and what are we talking about? And of course, like all of our kids were raised with us as nurses and many of them are in the medical field now. So it's just something that, it's kind of like a natural progression for some people, but, yeah. So fun, right?
[09:52] Tara: Yeah. So you're a better Catholic family than us? It's just three of us.
[09:59] Michelle: Yeah. There were two families in town, in the town where I grew up. So there was our family with eight kids and then there was a Mormon family with twelve kids.
[10:10] Tara: Wow.
[10:11] Michelle: And so it's like at school somebody would meet you and they'd say, oh wait, I know both of your brothers and your sister. Are you that Mormon family or the Catholic family? Life in a small town, ight?
[10:25] Tara: Yeah. That's awesome.
[10:28] Michelle: I know, right? Okay, so let's go through your nursing history a little bit. Well, let me go back. So you've been a licensed professional counselor since 1998?
[10:42] Tara: Yes.
[10:42] Michelle: And then a nurse since 2002. Then you went back and got your psychiatric nurse practitioner in 2009.
[10:50] Tara: Yes.
[10:50] Michelle: And so in there you worked in the ED. Was that as a nurse?
[10:55] Tara: Yes, I started actually as a sexual assault nurse examiner. I love it.
[11:00] Michelle: Okay.
[11:01] Tara: Yes. I'd love to even talk a little bit about that because it was interesting because people like, why do you do that? I felt that it was a very good fit for me because I could do counseling as well as nursing. And just the way I'm wired, I am one of those methodical, I can be fluid and I'm not so stuck on, I must swab this first. But it was just a very good fit because I'm methodical about how I do things. But it wasn't just cold and because I'm a counselor, it was a really good fit. Like somebody talked to me when I was a new nurse about it and I said, I think I want to do that. And my boys were really young and then I would do that on call and people would say, oh, so you're a nurse. What do you do? People think you're a pediatric nurse or a NICU nurse. I'm like, sure, sexual assault nurse examiner. And then the room gets quiet because I was on call and it just seemed like at three in the morning was usually when I get called in. And so now this was from 2004 to about 2009. Then along that time, then I morphed into an ER nurse. And I think somebody else was talking about this on your podcast, another sexual assault nurse examiner, and I'd love to listen to her. And she said it's not feasible for the nurse. I'm there scheduled to do my shift, but then I'm held up for anywhere from three to 5 hours with a sexual assault call. So then that kind of faded. We had it on call system. And one thing that we have regrets. I wish that I kept it up, but I didn't keep it up, because then I went on and I became a nurse practitioner, and then I had another job and I just stopped doing it. And now so much time has gone by, and I bet hopefully it's a whole new way to do it, because it was paper, pen, it was charting like that. We didn't even chartically. Yeah, it's kind of frightening. We didn't have the only thing I did during the exam that seemed to be like, I mean, it seems like the olden days, I would insert a speculum and I would put toluidine blue, and then we'd use a woods lamp, and that's how we would look for injuries. And now I'm sure it has progressed a lot more and there's more rigor. So that is how I ended up being a sexual assault, sorry, nurse examiner, what we call known as sane, into the ED. And it was a Level I trauma. It was a Level I trauma ED. So it was, you just are thrown in and it's like. But I'm the nice psych.
[13:52] Michelle: Heather and I, my guests for that episode, we were talking about that because, at my institution, that was exactly how the same nurses operated. These were nurses who worked primarily in pediatrics, labor and delivery, and the NICU. And so, yeah, working the NICU, it's like, hey, we have a victim in the emergency room, and you need to give your patients to someone else and leave your assignment for, like you said, up to 5 hours, 6 hours sometimes. And it wasn't feasible. We did that for a little bit, but then they started having them take call and stuff like that, and it worked a lot better.
[14:41] Tara: Yeah, because it's just like you're saying it's not feasible.
[14:46] Michelle: Well, that's such an interesting specialty. And I would imagine you were very effective because of the fact that you were simultaneously a nurse and a therapist. And in that realm, those two go hand in hand, and you can do a lot of damage to a person's mental health in that setting if you're not aware of what psychologically the victims are going through. So I would think that would be perfect for you.
[15:23] Tara: Yes, because I think what you just said was an answer that I give to people when I would do that work. They'd be like, why do you do that? And again, because it was like, I had small kids, like my boys when I started. I was actually pregnant with my youngest, who's now 18, and the other one was like, a little bit over two. Like, they're a little bit less than two years apart. And I said, because it's most likely somebody's worst day, and I am tasked with the start of helping them heal, and that's the way I looked at it. So, not that you want to say, well, it's an honor and a privilege to work with sexual assault nurse examiners, but I took what I did. I don't take myself very seriously, as you see on my Instagram, the lifting, but I took that job, and I take my nursing jobs. I do my jobs really seriously, because it all's like the same with anything, be it a NICU nurse, a pediatric nurse, a psych nurse practitioner, oncology nurse. We are vessels to help people heal. And so I take it very seriously what I do, and I do not take what I do lightly.
[16:36] Michelle: And I see that before you were a nurse, you had worked in foster care, a case worker. You were a mobile crisis counselor with your local police and a mental health therapist for child and adolescent psychiatry. And so I would imagine all of that experience going in, and now you're a nurse, you're just so much more effective at addressing all those mental health needs.
[17:05] Tara: I try. There's always a learning curve. And I think even though now I've been a nurse, what, for 21 years, a psych nurse practitioner going on 15, there's always something to learn. Also, when I want to say, just when I think I got it on lockdown, then something new is thrown in, whether it's medicine or even, like, a social issue that just kind of because I'm on a college campus, that kind of ripples through the community. We're always learning, regardless of our specialty, especially as nurses, we have experience, which is great, but I think when a nurse becomes dangerous is when they're stagnant. And when they say, well, it's always been this way, and you're not willing to say, well, maybe there could be a better way. Sometimes there really isn't. And there is, I think, a lot of value in being a nurse with experience, because sometimes, and I'm sure as the pandemic really highlighted this, you had this mass exodus of seasoned nurses, which is tragic. At the same time, even in my field, where there's really not a lot of new stuff, it's like we seem to recycle things and just call them different things. For example, what I mean by that is it seems like motivational coaching was, like, a hot topic for a minute. But really what it is is being somewhat engaged in learning how to answer questions. I mean, not answer, ask questions in a more effective way than somebody feeling they're on the spot. Being mindful, like, mindfulness takes off. But really mindfulness, when you think of it, is, we're trying to help people be in the present. I'm trying to think of some other things that will probably come to me or medication. Medication for a while. We see off label, hey, this works for this. And then finally they do the studies, and then they make it brand name, and then they charge such a ridiculous amount where it's like, come on, we knew this before. Like, a perfect example is Wellbutrin, right? Wellbutrin is bupropion. That's a generic. And we've used this for a long time for depression, for classic depression, where you don't want to get out of bed, you have dysphoria, depressed mood, lack of energy, all that. But also we saw, hey, it helps people not want to smoke and not vape. So then it was repackaged. And this was years ago, too, to Zyban. Nobody can afford Zyban. So it's just things like that that's so interesting.
[19:56] Michelle: Yeah. And I love all the off-label discoveries. Here's a perfect example. So the very first time I hurt my back, I was prescribed Flexoril.
[20:08] Tara: Right.
[20:09] Michelle: And so I started doing my research on Flexoril and found that it was actually being used off label as a muscle relaxant. But it was a tricyclic antidepressant.
[20:22] Tara: Yes. And, Michelle, I want to apologize. I'm not too sure. Did I answer your question? Because I felt like I went on a tangent.
[20:37] Michelle: Yes, but I want to delve deeper into where you are right now. So you are the sole psychiatric mental health nurse practitioner at the University of Arkansas at Little Rock?
[20:50] Tara: Yes.
[20:50] Michelle: And so I imagine that you work with students. Is that correct?
[20:55] Tara: Yes. A lot of people, or even sometimes I'll share our social media and people assume I'm in a teaching role. I'm not in a teaching role. I'm strictly in a clinical role. So what I do there is, and it has morphed over the years. I've been there since 2011, and so I do psychiatric evaluations, I prescribe medication, I also do counseling. And part of why I love working with college students, I also feel it's a privilege and a pleasure to work with that age group because there could be so much growth. They're not so far gone and rigid that they're difficult and they're out of their family's house. Because I used to be a working child adolescent, and that was rough because a lot of it depended on the kid's success due to parental or guardianship and the buy-in with the family. That was also school-based counseling. I know it is such a need for it, but I felt like that kind of sucked my soul. So I'm a fully independent nurse practitioner. Our state started to do that last year, and so I applied for it because I fit the criteria. Like, I've been a nurse practitioner long enough. I had to be endorsed by a medical doctor and then endorsed by our director, and then within probably a year later, then I was granted that. So because of that, and I take the position very seriously, there's things I could treat, but I just refer them off campus because we don't have the infrastructure for certain things. Like at this age group, psychosis is an issue. You could have your first psychotic break, but if those things happen, we have to send you off campus. I don't have admitting privileges into hospitals. And the way it is going now, with a lot of inpatient, we'll see students that are suicidal, who voice suicidality. And also there's certain diagnoses, like persistent depressive disorder. That's basically a symptom of it. More days than not, some of them really want to die, and they have persistent thoughts of suicide. And at times when I'll have graduate students with me, they're kind of like, oh, my God, are you going to hospitalize them? I go, but they don't have a plan, and they don't want to go. If they don't want to go and they don't have a plan, there's nothing I can do. But we just keep much more eyes on them and we help them through that. But the counselors do this too, so we're seeing a lot more of that on the college campus. So that's what I do. I do counseling, med management. I work on a team with all the other counselors. Our counselors are, either they go through a counseling program or a social work program. And we have a few doctoral students that come and we'll do a practicum and leave. But we're not set up to do any testing, so we don't do psychometric testing.
[23:56] Michelle: Did you notice a difference in the mental health of the students, like pre and post-pandemic? : Can you speak to that?
[24:04] Tara: Michelle, oh, yes. And also, I think I have a special place in my heart for COVID. I call them high school COVID kids because my kids were high school COVID kids, too. And when 2020 hit, and I remember this very clearly because I was turning 50 March 1 2020, I had a normal birthday. I was the only one in my family who had a normal birthday because my husband, he was born later March, and on his birthday, everything was shutting down. And then my boys, who were born in April and May, it was pretty much locked down. And then bringing that then, to answer your question, so one son was a junior at that time. So you saw 2020, which was really sad. These kids couldn't, they didn't have a high school graduation. They didn't have a prom. But in certain states, and also, like, it was part of Arkansas, where my kids went to school and they went to a public school, my son, and this was the class of 2021, and this is what we saw on college campus. They were coming in as freshmen, but they've not been in a class for a year and a half. So it was a lot of adjustment. And also I saw a lot of persistent depressive disorder where people say that's like it's old school dysthymia, but really that kind of minimizes it. It's like more days than not that they're depressed, they're dysphoric. They have a lot of negative thinking. They could have sleep issues and then the anxiety of coming back to class because there were still COVID cases. There was a lot of political issues about it and all that. And I remember in staffing, we're like, oh, we're seeing so many sick kids that go, wait a minute. Let's back up. This is what we're really seeing, is people are adjusting to a new normal. These were high school kids that missed for a year and a half. They missed dating, they missed prom, they missed graduate, they missed social interaction. And so it was almost like they were delayed. So we saw a definite uptick. And I think it was know. People think, oh, is it depression? Is the number one thing you saw. No, I saw a lot of anxiety. But interesting enough, Michelle, the ones that had seen me before that had social anxiety kind of thrived because they didn't have to worry about class because everything was online. So I was worried about them when everything started to open. But it was weird. The ones that were introverted did better. But really, and I don't mean that introvert. Well, you're introverted, you're going to thrive in a pandemic. But, the ones that had social anxiety did better than ones that liked to be out and about. And then everything shut down. And then it was interesting. I had one student, every day, the student wanted to die. And it was just like every time I'd see the student, I'm like, oh, I got to get you into a hospital. But they just wouldn't walk up and say anything that I could act on. But then this student was then diagnosed with cancer during this time, and then the suicidality left. And I said, wow, what the student told me, he said, now that I might die, I wanted to be on my terms. And then I have kind of a 6th sense of humor. I know who I can say this to and who not to. I said, it's like you've been training for this your whole life because I use a lot of sports analogies. And he said, sure. The student said, yeah, you're right. But COVID was very interesting working on a college campus because we had to do telemed and a lot of students would have to talk to us in their cars, in bathrooms, in closets. Yeah. Because obviously they needed to talk, but they were around family I could definitely speak to. I think mental health really came to forelight the forefront during COVID because I think everyone's mental health, I think it was safe to say, was trash. But some people did better than others. Some people definitely did better than others.
[28:32] Michelle: Yeah, it was a really interesting time. And I love how you made the distinction with the students that the ones that had some social anxiety kind of did a little bit better. And I found that true in myself a bit. I'm kind of a homebody. And lockdown for me was like, yes, I don't have to go anywhere. It was freeing. And I still had to go to work, which really sucked because there was so much on the news and even within our own institution, at least four or five times a shift, we had updates about how many COVID patients we were seeing and how many patients were waiting in the ED and on and on and on. It was just like overkill. And this was all like pre-vaccine.
[29:31] Tara: Oh, yeah.
[29:34] Michelle: And then the whole vaccine thing came out and I was like, sign me the fuck up. I want this. But it became very polarizing. I've said a lot of times that as nurses, we don't do it for the applause, right?
[29:52] Tara: Right.
[29:53] Michelle: And at the time of the lockdown, as nurses, we had never received so much from the community. It was like this community outpouring of love and respect and adoration, and companies and individuals were sending us food and gifts and they were hanging huge banners out. And we love our heroes, and we have to say that it was nice, right? We don't do it for that, but it was nice to be recognized for what we do. And then when the vaccine came, man, did it get crazy. And, yeah, there was so much just angst and anger towards the medical community. So just, man, such an interesting time. And I can't say that we didn't come out of it with scars, because we certainly did. But hopefully it'll be a learning experience for the next one.
[31:04] Tara: Right, Michelle, I think you said it perfectly because I definitely think there's some scars because, yeah, it tore families apart in a lot of ways. And I remember saying this to a colleague, I said, there's no telling the type of trauma we're going to. You know, people, you know, they were like, no, that, like the stuff that was going on behind closed doors with the students. Because people have also this misconception of working in college, mental health. They think it's because now it's politicized. Oh, that's the elite. I work at a university. It's a public university. We have a lot of first generation students. These are students also. A lot of them are on scholarship. And a lot of them, their parents or guardians are either unable or unwilling to really help them. So they're financially on their own. A lot of them. They're not just sitting around like, oh, I guess I'll go to class even. These are our traditional students. They are working hard. A lot of them are scholarship, yes, recipients. And then to come here and try to navigate a lot of this stuff or just navigate the health system and then, like, what you're saying with the vaccines. Because I am a psych nurse practitioner, I stay in my lane. I don't deviate. I stay within my scope. But because it was so hard to access care and I would be seeing a lot of these students on telemed, they would tell me their medical problems, and I appreciate my scope, but I would try to help brainstorm some of it, or they would fall off of care, or then even I didn't know any better than anyone about the vaccine just to try to help them make an informed decision. But I had to be very careful because it's like, well, you can't talk to them. It's like you can't win either side. Sure. And at that time, you probably saw on Instagram, I would still compete in powerlifting meets, but I'd also be nervous because I also lived around some high risk people. And then I don't know if D.D. was telling you this, but in 2020, she's our half-sister, but a sister nonetheless. So our father had lymphoma. He survived and he's fine. But at the same time, we had a sister who had breast cancer. I mean, not breast cancer, I'm sorry. She started with ovarian cancer. It was treated, but then she ended up having stomach cancer metastasized. So at the same time, and this was in 2020, all this was going on, I had to go up to Boston because my mother also had surgery, too. So I had my mother having surgery, my dad diagnosed with lymphoma, a sister who was all of a sudden with stage four cancer and then trying to do my job. I'm pretty good at compartmentalizing but interesting enough is because I was sitting so much, and I'm a person who likes to move like I'm sitting in a chair talking to you. But I've shifted throughout this.
[34:03] Michelle: Sure.
[34:04] Tara:I started developing all this joint and bone pain because just sitting there and being so tense, the perfect. And it's not perfect, but I guess the best example of what was it like being a mental health provider during that time? Because I feel I have it a lot easier than the people who worked in the hospital, because I didn't work in a hospital and I was safe in that way. But back to the powerlifting thing. I'd wear a mask at certain meets. And I know people, nobody gave me a hard time because they knew I was a nurse. And I think some people also knew my story. Know, I was kind of going back and forth from Boston to know Arkansas. But also there was a lot. I mean, people would come to me and be know. But what do you think? But it was just so politicized, Michelle. And it was like you just couldn't. And I just tried to stay neutral. I tried to the whole thing, but it was a really rough time. But I think the perfect example, if I could give you being a mental health provider. And just managing everything was. So then my sister ended up passing away. She was in another country. She was raised partly in Thailand, and then she was raised in the Netherlands. And we couldn't get over to see her because the borders were closed. And so I had to watch her funeral online. I let everyone know, hey, give me an hour so I could watch this funeral. And at that time, one of the students that I saw attempted an overdose in the dorm. So EMS was called, and this student was awake and alert, but said, I'm not going, but I want to speak to Tara. So everyone's getting on the phone with me. And I said this. I need 20 minutes or I will lose my job. Let me do this. I will be there. Handle it for 20 minutes. That, I think, was the perfect example, if I could show you of what it was like to be a mental health provider during that time, because also, everyone who I worked with, everyone I worked with, one person lost a mother to COVID. Everyone had stuff happen. And I'm sure with you, everyone had stuff happen, whether you. So we all were in this together, is what I'm trying to say.
[36:30] Michelle: And just listening to your story right there, how you said, I thought I had it better than the nurses that worked in the hospital. And I immediately thought, oh, no, because I think yours was much more difficult because you're handling the mental health aspect of it. And some of those things are, to me, looking in would be so difficult because you don't affect change like that quickly in mental health. Whereas if I'm a nurse in a hospital and I'm taking care of a patient with COVID that's a much more active role. I feel like there are so many more things that we could do intervention-wise, to help the patient. But that's just my perspective from a nurse that's worked in a hospital. But the mental health thing is just so huge, and I would imagine so many times just feeling helpless. Do you experience that?
[37:35] Tara: Yes. And thank you for saying that, because I do really appreciate it was definitely not easy. And then it was kind of like, as a mom, I'd be worried that I wouldn't have anything to give to my kids because I knew, like, everyone, these are high school students, and they were one day in class and the next day trying to adjust to learning online. Just not even just the educational component, but the social component. Like, one of my kids was, like, a wrestler. He couldn't wrestle, or it was just things like that. And I'm not speaking like I'm unique. We all went through that. But I think what really helped, as I said, that's when I started my little Instagram stuff. I did my little silly reels. Thank you. And I think it was just, even though it was never really about my job, it was just about lifting. It was almost like I had two separate lives. I could be Tara, the walking deadlifter. This lawn lanky, doesn't look like a powerlifter, but competitive power lifter. And my silly shenanigans versus the nurse practitioner who's seeing students. Just some of them. It was just like, just trying to honestly keep them from hurting themselves.
[38:52] Michelle: Yeah.
[38:53] Tara: As we did here over and over, just a lot of students with dysphoria. I also worked with several because I'm on a college campus, a chunk of nursing students who are then just thrown into. Can you imagine being a new nurse? Barely a new nurse, and just thrown into ICU, thrown into the ED with no experience, and they're just learning it on the fly and what they're seeing and then just what they're dealing with as a 22, 23-year-old and trying to navigate society and all that.
[39:27] Michelle: Yeah, I remember during that time, because we have a local nursing school and they do clinicals in our hospital, and they shut down clinicals, and these students were going to labs to try to learn how to take care of patients. And those graduating classes were just, like, at a loss. They're like, well, I've never actually seen this in real life. I've just experienced this in a lab, and they missed out on so much.
[39:59] Tara: Yeah.
[40:01] Michelle: Well, we're going to switch gears here for a minute.
[40:03] Tara: Sure.
[40:03] Michelle: One of the things I saw in your bio is that you're currently back in school to be an EMT Basic? Is that correct? You got to tell me about that?
[40:22] Tara: Sure. I think DD I've always been fascinated with emergency medicine. I don't think I'm well suited to do it because the way I am, I'm methodical. I loved working in the ED, but also, you also get thrown into so many, you have to multitask fast. Where also, now what I do is I sit, I listen to people for 30 minutes to an hour. I'm fully engaged now I'm going through a triage system in my brain, and I'm thinking psychosocial, and behavioral. Is this a medical issue? Is this something that could work out with counseling? But no. Yeah, it's nothing like first responder. And I thought, I'm 53, I'm still in good shape. I was just telling you, I think really what stuck out was having going. I told you about 2020, then 2021. My mother and father were both hospitalized in a hospital up in Boston. My father had COVID, and my mother had a nonfall hip fractured, peripherated an ulcer, and then had a pulmonary embolism. You cannot kill her. She's still alive, okay? Like, she's very tough. But going up there, because they literally, one was hospitalized, discharged, and then the other one went in and then taking care of my mom and then going in and see my dad and going back and forth, back and forth, back and forth. And at the same time, Michelle doing telemed across state lines, which now we can't do. But it was just so I was working, but at that time, I was just like, I don't really know anymore what to do in an emergency. And really, response time obviously was slow because I also spoke with EMT and paramedics during that time because some of them were taking prereqs and then just listening to. Even though DD was doing flight nurse, hearing the first responders and all that they were going through, felt, even if I had never formally been hired at an ambulance company and did this as a side hustle, I wanted to go through the training because also as an ER nurse, it's a different perspective, but I felt like I lost all those skills, like how to triage trauma, even though it's different in the field as an EMT versus you're an ER nurse. So it was just kind of like, I hate to use the word calling, but I felt it's time. It's time before I get too old and have difficulty doing the skills or too much brain frog, excuse me, for menopause. Can't retain it. So I even asked to go, am I the oldest student you ever had? And he said, well, no, there's a 70-year-old that's there with his grandson in another class. But half of the students are obviously, I'm old enough to be everyone's parent in that class. One student, we were just kind of sharing social media, and I saw a picture of my son, and he went to middle school with my son. Wow. And then I gel really well with the firefighters because not that I was ever a firefighter, but we have that shared history in a sense of, because when I worked mobile crisis, especially of being, in a sense, on a scene and seeing things and also being a counselor and a nurse, so I would not freak out over stories, I would listen. I was, I guess maybe a safe place to debrief. And now it's personal. I want to pass this class and I want to sit from the National Registry because I have a solid A in the class. But what's been implemented, and it's a lot like nursing school. When I was in nursing school, right at the end, they implemented a policy where you have to pass the Hesse. No matter how great your grades are, if you don't pass this Hesi, you don't get to sit for the NCLEX. And so what they're doing now is know we have tests that we take that is based on the book Pearson, which is like a big EMT book, but now we have to pass adaptive tests that are national. And if we can't pass those tests and it has nothing to do with our grade, we can't sit for the National Registry. And Michelle, this is personal to me now. I want to sit on it. I'm on a mission. I am going to get this done. [44:57] Michelle: Well, I have so much respect for just what you did, like seeing a deficit or an area of your practice that you feel like you need more experience in and then doing this. And it's kind of a hard concept to get across to students, nursing students and new nurses. And I've been a mentor to both. I taught clinical for, gosh, twelve years with my local nursing college. And I would have students and nurses say to me they would be avoiding certain things.
[45:45] Tara: Yes.
[45:46] Michelle: And I'm like, why are you avoiding that? Well, I don't feel comfortable. I don't have enough experience. And I'm like, okay, then it has to be your mission to do that over and over and over again until you feel comfortable. So if it's IV sticks, come on at the beginning of your shift and say, hey, anybody that needs an IV today, call me. I'm the person. Call another unit. Hey, I'm over on this unit. If you guys need IV help, call me. I'm going to come and just do it so many times that you get good at it. And so I just have so much respect for that and especially where you are and with all your other credentials. Just saying I have this area of my practice that I feel like I need more experience in and then just doing that. And you just probably have such, well, obviously you have such a competitive side, but you're competitive with yourself.
[46:51] Tara: Yes. It's like, this is on. I'm like, this is on. We're going to pass this. And also the other thing, when people say, why are you doing this? And this is true and probably unpopular. I said psych nurses were useless in medical emergencies, followed closely by psychiatrists, but it's kind of true. And again, I saw that with the health issues that my dad was having and then my mom and then literally being up, spending extended time in a hospital, because then I started worrying also when I get older and then certain things that then just as a nurse, I'm like, okay, when they have chest pain, am I supposed to give aspirin or remember, like hot, dry, sugar, high, cold, clammy, give them candy? Like those small things, do those things still apply?
[47:44] Michelle: What's the current research say on it?
[47:48] Tara: Exactly. And then the other thing too, where maybe it's serendipity, but I'd be that person. I'm off. I'm just going to a grocery store. I'm just driving home. I would roll up on some. I live in our capital, our state capital. I've rolled up on just about everything but a gunshot yet. But as in the first person, one of them, the boys were young. It was a woman who was hit by a car. I believe she was intoxicated and probably under the influence of drugs because then she was trying to get up, walk, and she was trying to. I pulled over and I was praying, please, boys, don't get out of the car. And she was dressed in black and she was covered in blood and she had an open fracture. And then the woman that hit her, she didn't see her and she was a mess. So it's like, okay, she needs to be taken care of, too, because she's screaming, crying. Then it was like I had it together to call. But I also knew this woman is going to make. This woman who was just hit, she could move and really hurt herself. So I sat with her, tried my best to splint, but I had nothing. So it was things like that. Or I went into a grocery store and somebody had. I walked right in and the person was ahead of me. And then he dropped and had a grandma seizure and start thinking, you know, even it just seems like I'm that person. So I probably need to go back and learn some things. So that's my story.
[49:21] Michelle: I love it. I have so much respect. That's awesome.
[49:26] Tara: Thank you. It's hard. It's funny because. And this is why it's hard. I really like EMT, basic training. I really do, because it fits well. We learn a different perspective, but a lot of it, it's not hard, but it's just like in nursing school, a lot of information. And when you're 53, your brain just doesn't work quite as fast. So I talk fast and think fast. What will happen is I work a whole day of doing what I do, then I rush off to class and I'm good for about a good 2 hours, and then just my brain shuts down and it looks like I'm answering questions. I know what I'm doing. Then guess what we're going to do. Skills. And then it's like. And my brain will get stuck. Was it a dressing or was it a bandage? Or. I'd say over and over in ahead. I mean to say put on a pelvic binder, but I'd say pelvic girdle. And they're probably like, yeah, I'm sure this woman worked in the ER. I'm sure she's a fully independent nurse practitioner.
[50:34] Michelle: That's great. Yeah, it humbles us, right?
[50:38] Tara: Yeah.
[50:40] Michelle: When I went back for my bachelor's, let's see, I was one month out of my final chemo treatment for breast cancer.
[50:50] Tara: Wow.
[50:51] Michelle: So did I have brain fog? Absolutely. But was I motivated? Yes. Because I thought, you know what? I just survived breast cancer, and if I don't do this, the time is going to go by anyway and I might as well just do it. It was like an 18-month course, but my first class was damn statistics. The thing that all nurses, I think there have been studies that nurses don't go back to school to get their bachelor's because statistics is so intimidating.
[51:28] Tara: Yes.
[51:29] Michelle: And, man, it was hard. About three weeks through, I thought, I'm going to have to drop this class. I just don't get it. I just don't get it. And then it just like something in me clicked and I was like, hell no, I'm not dropping this class. And I got an A and then my first A. Yeah, right. It's like it catapulted me into, okay, my next class, I'm going to get an A in that, and I'm going to get an A in that, and damned if I did not get straight A's through my whole program. So, yeah, I was really proud of that.
[52:05] Tara: Well, I'm proud, too. And also let's appreciate just also the trauma of having cancer and then having to go through chemo, because cancer is cancer. But then there's cancer. Like, then there's breast cancer. Could be treated with a biopsy and radiation or just a biopsy and a pill versus hardcore chemo.
[52:29] Michelle: Mastectomy, chemo, five months, all of that. So after that I was like, all right, I can do hard things, so I'm going to do this. And you know what? It wasn't that hard. Compared to, well, talking about doing hard things. I want to talk about you being an athlete. I want to talk about Tara the Walking Deadlifter, because I'm impressed. I instantly connected with you on that level because I told you I did two years of CrossFit, and I have the utmost respect for athletes of any kind. And that community, oh, my God. Just the love and outpouring of support, it's what I needed. I was a couple of years out. My husband passed away in 2016, and I know I was still grieving. And my sister said, hey, so she'd been a crossfitter for a while already. And she said, hey, why don't you come to the friends and family night and I want you to see what I do. And I was like, sure. So I credit her for tricking me because I went. And the coach, who was just a gem, he was like, hey, do you want to get in here and do a session? And I was like, yeah, sure. And I did my first CrossFit class, and it was hella hard. But from then on, I was like, this is awesome. And he was like, see you tomorrow. And I came back the next day, and then I signed up. So just knowing that that's what you do and the heavy lifting and doing hard things, talk about being an athlete, and what does that do for you physically and mentally?
[54:29] Tara: Sure. First of all, I want to say that is amazing that you got into CrossFit. And again, I'm very fortunate my husband is still with me, and I can only just the grief of going through the loss of your husband, and I'm so glad you found CrossFit in a community.
[54:47] Michelle: Yeah. Thank you.
[54:49] Tara: To help you through. It's so I never stopped working out, like, when I lived with basketball players when I was in college. And so when I stopped running track, I would still run, and I would run when they were playing basketball. And I look athletic, but I'm not coordinated. I would have been a point guard. I was a little bit over five seven at the time at Law and lean, and they were like, oh, can she play basketball in my room? It's like, no, she can't because I still would run. And then my boys were born, I'd run, and I always lifted weights. I lifted weights since I was a teenager, but I didn't know what I was doing. And then it was D.D. that actually kind of talked to me about CrossFit but I liked the heavy lifting more than the CrossFit. I liked the deadlift. With encouragement, I entered my first competition in 2015, and I didn't know what I was doing, but then I had newbie games, and I watched YouTube, and I competed in one federation where I ended up, there's so many federations, okay? So I don't want to make it sound, like, much embellished, but in that federation, I set a world record in deadlift, and I never had a coach. I learned how to do it from YouTube. And you have drug tested and non-tested, and I don't use performance enhancing, but it was a non-tested federation. And then I went into another federation that was drug tested, and it was only in the deadlift, but I set national records that. But also, there wasn't a lot of us. There wasn't a lot of us. And I'm also tall for my weight class. Like, when I would go and it was kind of fun because people look at me like, yeah, right. And then I would deadlift it, like, whoa. Because I think it's just left over from track. But then what happened? And I'm coming out of the end of it. You peak. And over the years, I've gotten stronger. Where I could do sets of threes, sets of fives. I have really good muscle endurance, which really doesn't help in powerlifting. You need raw strength. But the only thing that I've gotten better in, strangely enough, was the squat when, though I was diagnosed with cervical spinal stenosis of a cystic lesion on C Five, which kind of scares me sometimes because I know C three, C four, C five keeps you alive. And my SI joint, my right shoulder, basically on the right side. Skeletally, even though I'm 53, it has degenerated to that of somebody 25 years older. So late 70s, early 80s. But guess what? My bone density kicks ass. So I am motivated to keep going. But I had to go through where powerlifting has really taken off. It's a great community. A lot of older people are doing it. But no, I can't compete against young people, in all honesty, even people in my age group. I mean, these women are kicking ass. They're coming in, and you have to appreciate, and I don't want to make excuses for myself, even though I'm their same age, but I've taken so many dings from years of running lifting that I am probably not going to get much stronger. I do have a coach and my coach and everyone also around me, like, well, you need to put on weight, but there's just so much weight I can naturally put on. I didn't even have to cut weight last time, but it's also because of stress. I wasn't eating enough. Now I can eat like an asshole, as they say, and put on a bit of five pounds. But the context for a powerlifter. I compete as a 60 kilo, 132 pounds, but I'm over 5'6, so that's not like model skinny. But for a powerlifter, a lot of the women who are in my weight division are at least a good two, three, or four inches shorter. Like probably my height. You're seeing anywhere between the 148 to maybe even heavier. That goes up well over 200 pounds, who just are filled out more proportionately. So I look like a praying mantis when I deadlift, just like limbs, but I don't hurt doing deadlift now. Bench really hurts me because of my shoulder, and I've had a lot of issues, but I think why I keep doing it is for the health benefits. And I also like to compete because I think it's good. It kind of gets you out there, though. It's not as fun anymore, and I hate to say it, it's not as fun anymore because I'm not winning. So then I had to readjust. Well, okay, it's okay if you don't win. At least I can at least break PRs, my personal best.
[59:57] Michelle: Exactly.
[59:58] Tara: So that's what keeps me going when it comes to competition. But also, in a weird way, I think this also helps me connect with student athletes because I get it as an 18, or 19-year-old, being great in high school than going to college and trying a college sport. And then I get it also too, when you're injured. And I also get too, when you have to start to shift your focus of your why when you're no longer winning. And even though I'm in my fifties and I'm not young, they don't have to worry about that. I don't want to put my issues on them, but I think I'm pretty good at helping people adjust and finding a different why. And that's one of the reasons why I do my little, as I say, I'll call them trash reels to help people find their why to keep moving. Because seriously, even though I have a lot of these joint and bone issues, I'd be a lot worse if I didn't.
[01:01:00] Michelle: You know, I love your competitive, you know, the way CrossFit works. Obviously you know this, and I experienced this a little bit a few months into doing CrossFit because I could never do anything strict, so I couldn't do strict pull-ups. And so I did ring rows. I had to scale everything. And I started really feeling just this impostor syndrome, like, what am I doing here? I'm not an athlete. I'm overweight, I'm out of shape. I'm deconditioned. And it took another master athlete. So one of those older athletes who had been there, like, I don't know, 15, 18 years, and he gave it to me straight. And he's like, no, don't look around at all these other athletes. Like, you are also an athlete.
[01:01:59] Tara: Yes.
[01:02:00] Michelle: And the only person you need to compete with is yourself. And started talking to me about PR'S, and I started keeping a journal, and I started on the deadlift. And I will say, and you're going to laugh at this, but my personal deadlift best by the time I had stopped was 105. And for me, that was a lot because I had started at, like, I don't know, 50 or 65 or whatever, and it took quite a while to get up to that, but it's true. And we compete with ourselves. And when we do that, when we find our personal best, it's like we are still winning. We are winning in a different way.
[01:02:50] Tara: Well, I want to say, if anyone was to laugh at you at your best, they're pos. I would never laugh at anyone. And you are an athlete. You're moving. You're moving. And if I had my way, I would want you to keep deadlifting because would you think of getting back into it?
[01:03:15] Michelle: I think about it all the time, and I'm just like, you know what? If you're thinking about it all the time, do it. And you need to do it. You need to get back to it.
[01:03:25] Tara: Yeah, do it.
[01:03:28] Michelle: I know. And I know all the benefits of bone density and lifting heavy things. And I recently read Laura Kudari's book, Lifting Heavy Things, Healing Trauma one rep at a time. Yeah. So good on so many know, because she had directed it towards, she had always been a lifter, but then when this thing happened to her in her life, where she was experiencing, like, lifting, actually helped heal that trauma so good. And then the other book, of course, anything by Kelly Starrett is amazing and Built to Move: The Ten Essential Habits to Help You Move Freely and Live Fully. So those are my two latest books on lifting and athleticism. Do you ever prescribe movement for the students that you counsel?
[01:04:29] Tara: I tell them all about exercise. Like, in my office, I have all my trophies, awards, and certificates, and it's not like to brag but to show. I'm like, hey, you don't even have to be on this level. And pretty much I say the same thing. I go, I'm not asking you to run a marathon. A tough mudder, which D. D. and I did together, by the way, in fun or Powerlift, but we got to get you moving. And I know you're depressed, and here's the crazy thing. You're depressed, so you don't want to move, but now you're even more depressed because you're not moving. And I have a barbell and bumper plates in my office. Michelle, sometimes I'll whip them out, and we'll whip them out, and I can show them how to do it. But I brought them there because I have a colleague, and she never powerlifted. And she came to me, she goes, will you teach me how to power lift? I said, by all means, I'd love to. So I still have my barbell and my. The bumper plates, and I talked to my director. I go, what do you think we do? Like, could we put on some deadlifting seminars? And so we've done two campuses at two different. We did it at the nursing school and in our art school, we call it, like, deadlift to destress, where we show them how to deadlift, and they go and we give them prizes, but it's not a competition. And we show them how to either do the sumo or the conventional, and they get in there and practice, and it's the coolest thing, seeing people never do this before, feel powerful. And we're not trying to do 400, 500, 600 pounds, but just move. And when people even do their own body weight, you can see it makes them feel really like. It's almost like. I think in some ways, I'm more sustainable and healthier than giving. Well, I can't prescribe Adderalls. I cannot prescribe stimulants on a college campus. And I don't prescribe opioids because it's not mine. But I'm not giving them, like, an immediate Xanax opioid. It's a quick, like, you're saying mental health is not a quick fix. Movement helps, though. Movement helps. It really does. And movement is going to help faster than a lot of the other. Some of the talk therapy and certainly medication, though at times, medication is, I think, for a chunk of people, necessary, but for a lot of people, they would do much better with exercise.
[01:06:57] Michelle: So underrated, right? I think we just jump towards pharmaceuticals. There's a pill for that, and it's like, let's make exercise the pill for that. And like you said, there are times when medications are warranted for sure.
[01:07:18] Tara: Yes.
[01:07:18] Michelle: But it's like, let's start with this least invasive, most helpful way to mitigate some of these things in the short term, and then we can work on the long-term things. That's so cool that you have those things in your office. And, wow, what a benefit to the students there.
[01:07:39] Tara: We're hoping next semester to do more, to do more of those. And also, our director, he started because he saw the benefit for him himself, personally, to something we call Movement Monday. So every Monday, they get a walking group together and walk and walk and talk. And so we call it Movement Monday. And so we, in our counseling services, that's where we work. We're definitely show. Also, we have yoga now. Like, we're trying to get out there, movement in whatever it is. Because I appreciate, though, I'm all about weightlifting. It's very intimidating for some people. And also we have a university weight room and students a bit like, hey, I'll take you there and teach you how to use things. So I've done that before. We've done that before, too, because the gym can be a scary place for people, and we want to show it doesn't have to be so scary.
[01:08:39] Michelle: Yeah. Wow, that's great. I love that, your Movement Mondays, we have something in our town, and it's run by our local hospital. It's called Walk with a Doc. Yeah, it's really cool. And so they get out and they go to a track, and the doctors out there and they can answer questions, and they're all just walking miles. Yeah, it's very cool.
[01:09:09] Tara: Oh, I like that concept, too.
[01:09:11] Michelle: Right?
[01:09:11] Tara: Walk with a Doc.
[01:09:16] Michelle: Well, what I want to know as we get ready to close is, so you're a counselor, you're a mental health practitioner, but I want to know who counsels the counselor. What do you do for your mental health? Who do you talk to? What do you do?
[01:09:40] Tara: It was funny because my instructor, my EMT instructor, one day, he's like, so what do you do again? And I told him, then he goes, then you come here? I go, yes. He goes, what do you do for your depression? And I told him, I go, I don't really get depressed. I get irritable. But what I do, obviously, is the working out, and I'm very structured. Honestly, it's kind of a bear. I lose my shit if I can't work out every day. I have to move somehow. Like, I wake up early and I work out before you and I. Today was leg day, but talking, yes, I do have a really good. I'm going to do a better job. I want to reach back out to friends, but what I've kind of done is, like, I'll cocoon because I've just been so focused on school and my job, and that's not always healthy. So I have support at work. We have a health service, and the director and I actually went to nursing school together, and she's a dear friend. So we'll meme each other and text and we'll call. Because, you know this, Michelle, sometimes you just got to debrief with a nurse that you really trust and, you know, it's not going know, say shit. And has got your, you know, my girl Chanel, so she's one that I debrief with. My husband is very rational and calm. He's a very good person when I'm feeling, like, overly emotional to talk with. And also, in fairness, like, all of us who are mental health therapists, we've all been in counseling at some endpoint. And so I've spent a little time on the couch myself. I haven't gone in a long time, but I feel like that's what I do. You have to have some people you trust. But I do know next year, 2024, especially, I want to reach out and have more reciprocity in relationships where it's not just like we're bitching about work. I want to be able to get out and do things and have fun because it just seems like it's work, school, and then. Not that we're bitching, but just like, debriefing. I don't know what it's like. I'd love to go out to lunch with a friend. I powerlift, and that's actually my social life, is. I'll wrap some meets, I'll go watch meets. But sometimes, because, again, sometimes powerlifting, especially when you're competitive, I'd love to get out in nature. Really? That's one thing I'm craving, getting out in nature more.
[01:12:17] Michelle: Yeah. And I think when D. D. and I talked, he was like, that's kind of like his soul food is like getting outside, getting into nature, and it's so healing and so beneficial and so completely underrated again. So I'm glad that you're getting that message. Wow. You are just. You're amazing. And I knew you were going to be. Yeah. First of know, thank you. So much. Yeah, you came in good company. D.D. was so much fun to talk to. D.D. such great experiences and just like, I feel like maybe there should be like a movie about your lives or something because you're both so entertaining and so knowledgeable and you've just been such a joy today. So I just thank you so much for coming on.
[01:13:18] Tara: Thank you, Michelle. I thank you for having me and also just knowing your story and what you've been through, like cancer, know, going through the death of your husband, and hearing you're from a Catholic family. I know about that, you know. So I appreciate what you're doing for us. I do. If I have like one minute to tell a funny Tara/DD story. DD got me into obstacle course races. So before I power lifted in my forty s, I was running obstacle course races and I was kicking ass. I was like usually winning my division and even placing open. And how I got into obstacle courses is D.D. and I ran one together ten years ago. And I would kid and tell people, the reason why we do this is we're reliving our childhood. I'm eight years older, he was eight and I was ten. And our father said, don't light fireworks. I'm like, let's go. So we went to our elementary school and we were lighting off fireworks and then the cops came and just like, because it's an open field, just like we saw the cop car coming and it was like, shit. So I'm grabbing his hand and we are sprinting and we come to the playground and there's a fence and I throw him over and then I scale it. I still have a scar, Michelle, from it. So I said, instead of a life of crime and criminal mischief, D.D. and I became nurses.
[01:14:49] Michelle: Great story. Oh, my God.
[01:14:52] Tara: Yeah. So I'm the oldest and he's the youngest. And we have, as I said, our sister passed and she's 20 years younger than me. But me, D.D., we have a middle brother. So us three were raised together. Yeah.
[01:15:05] Michelle: So fun. I see so many parallels with your family and mine. So great.
[01:15:12] Tara: Well, let me share that story.
[01:15:14] Michelle: Thank you. And D.D. never told me that he was into CrossFit or anything, but when I saw his picture, I was like, I think this guy probably lifts.
[01:15:26] Tara: I think he's getting more into Brazilian jiu-jitsu. He and his wife are getting into that. But yeah, he lifts and all that good stuff, too.
[01:15:35] Michelle: Yeah. Very cool. Well, you know, at the end, do the five-minute super fun. So let me set up my timer, and we will just go. Okay. Would you rather go surfing down a huge sand dune or relax in a hot spring?
[01:16:00] Tara: Oh, my goodness. Relax in a hot spring? Yes.
[01:16:04] Michelle: I'm with you on that.
[01:16:06] Tara: I'm just too old. You know what? If you asked me that 20 years ago, I would have said that, but now I just think, oh, Tara, that's just a fracture.
[01:16:16] Michelle: Okay. If you could make one of your hobbies into a profession, which one would it be?
[01:16:23] Tara: Oh, wow. I have been asked over and over, why don't you do personal training? You should do this. You should do along the lines of that. But then I think I would lose my passion. But what makes the most sense would probably do something fitness-related. That would make the most sense.
[01:16:41] Michelle: I could totally see that.
[01:16:42] Tara: Yeah.
[01:16:43] Michelle: Would you rather wrestle someone 50 pounds heavier than you or face professional players in a rugby match?
[01:16:55] Tara: Again, I think this would be a different answer. 20 years ago when I was faster, I think now probably a wrestler. And what I would do is just try to keep myself limber enough so when they lock me out, I can at least hold it. I will make it difficult for them, though I would like to believe that I still am spry enough to make it a difficult match.
[01:17:23] Michelle: I could totally see with your long legs, like, how you could get them locked in.
[01:17:28] Tara: Yes. Can I bite?
[01:17:32] Michelle: Biting allowed.
[01:17:34] Tara: Yes.
[01:17:36] Michelle: Who was your best boss and what made that person the best?
[01:17:40] Tara: Oh, wow. I'd have to say it's my current boss. The reason why he started as a counselor with us and really worked his way up, and now he's our director, so he knows what it's like to be in the trenches and I've never had a boss like that. He always asks for our input, and he will even work with us, ask our input in person, but then also behind closed doors because, you know, usually in a group setting, you don't always want to say your input. Definitely. And also, he has really advocated for all of us to make more money because we're in a university system. I think people think we're loaded. But all of us, not just me, all of us could leave and make two to three times the amount of money we make now, but we stay because we love it. And he knows that, you know this as a nurse, like, you'd have to give, like, a month's notice to leave. It's just those small things. So I think it's my current boss, definitely.
[01:18:47] Michelle: He sounds fantastic.
[01:18:49] Tara: He's a wonderful man. Yeah.
[01:18:51] Michelle: Would you rather be a professional polo player or a professional bowler?
[01:18:57] Tara: Oh, wow. And when we say polo, do we mean on a horse, not the water? Yeah. Oh, bowler. Definitely. I just think of fractures now. Now in my EMT class, I think, yeah. That's a trauma waiting to happen. Yeah. Bowler.
[01:19:15] Michelle: Oh, my gosh. What's the one thing you wish you had the money to pay someone to do for you?
[01:19:21] Tara: Oh, wow. Because I'm kind of a control freak. I have a friend that I pay her to clean my house, so that's huge. And she's a friend of mine, so that's huge. Yeah. So I really can't think of it. You know what? Making phone calls now and dealing with customer service sucks. And I think I'm a very pleasant person. I'd pay somebody money to do that.
[01:19:53] Michelle: Gosh. To sit on hold. Yes. Wow. We need to set something like that up, right?
[01:20:00] Tara: Yes, we do.
[01:20:02] Michelle: Would you rather win front-row tickets to the Super Bowl or play a one-on-one game against your favorite athlete?
[01:20:10] Tara: Oh, my God. Number two. One on one against my favorite athlete. Yeah.
[01:20:14] Michelle: I was wondering if. Because you guys are from Boston.
[01:20:17] Tara: Boston. And I know my family's not going to be happy with it, my father is going to be like, what? T? What? You ruled a chance to go to Foxborough, right? Wherever. Yeah.
[01:20:30] Michelle: Oh, my God.
[01:20:32] Tara: He'd be like, gee, thanks, Tara. Nah.
[01:20:36] Michelle: Right? Last one. Would you rather have Korean barbecue or Thai food?
[01:20:42] Tara: Oh, Michelle. Thai. Oh, my God, please. Thai food. Oh, I love chicken curry. Love basil. If I could. I love Thai food. So my son and I, the younger one, when he was looking at different colleges, that's our thing. We would go, like, every single city we went to, it wasn't a whole lot, and it was all down in the South. Our mission was to find the best Thai food restaurant. Wow. Yeah. So we went to, well, Albuquerque. That's where he's at college now, but go. We went to Huntsville, Alabama. Kansas City. I know.
[01:21:18] Michelle: Can you find good Thai food in those Southern states?
[01:21:21] Tara: Yes, we would go on Yelp. Yeah. Thai food, definitely.
[01:21:28] Michelle: So good to know. Yeah. When my daughter and I travel, we're all about the food. We don't even want to find what museums are in this city. It's horrible. We're like, where's the best restaurant? Food is life, though, right? Well, you did really well. I love it. That was really fun. So thank you for giving our listeners your off-duty side. Thank you. And thank you again, Tara, for being here and just sharing all your knowledge and your experience and your stories. Those are awesome.
[01:22:04] Tara: Michelle, thank you so much for having me and I hope when you play back I wasn't rambling too much because I could get on a tangent. Thank you.
[01:22:13] Michelle: Yeah, you're awesome. I love it.
[01:22:14] Tara: Thank you so much. Not just for having me but for what you do and highlighting other nurses because I've listened to like I get on a roll like when I drive and I'm like oh, I can't wait to hear about the hospice nurse. I'm almost like oh, it's now time to listen to the nurse that sells real estate. So I mean I love your podcast. Thank you for what you do.
[01:22:33] Michelle: Thank you so much. I am having really the time of my life. I'm having a lot of fun so I appreciate that. Well, I'm going to get outside and do some movement that you have a great rest of your day. Tara, thank you.
[01:22:48] Tara: You too Michelle. I appreciate it.
Podcasts we love
Check out these other fine podcasts recommended by us, not an algorithm.

Two Humerus Nurses Podcast
Kelly & Alisha
Nine One One Nonsense
Sam's Pursuit
The Daily Stoic
Daily Stoic | Backyard Ventures
Essential Ethics
The Royal Children's Hospital, Melbourne
Behind The Shield
James Geering
Rapid Response RN
Sarah Lorenzini

