CancerSurvivorMD®
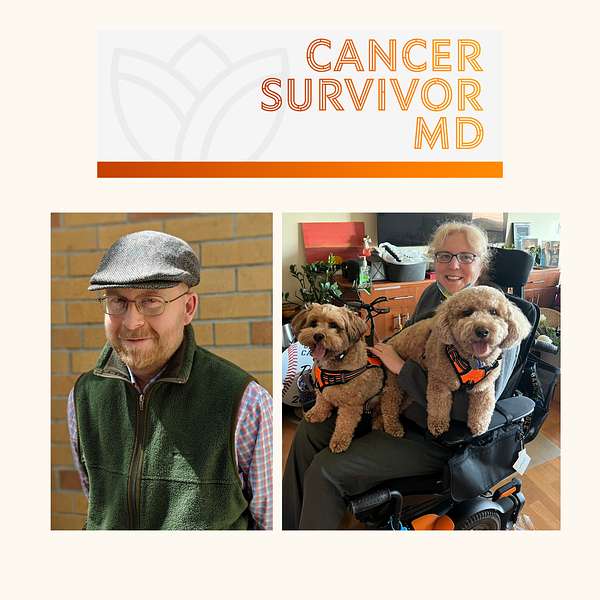
Hello! Welcome to CancerSurvivorMD’s podcast by Brad and Josie!
We will share our experiences with living in sickness, health, and anything in between to allow healing and growth. The topics will focus on cancer survivors and caregivers but will likely resonate with anyone who has been diagnosed with any health condition.
Brad is a retired English professor and cancer survivor, now a facilitator of the Writing as Healing workshop.
Josie is a retired medical oncologist and cancer survivor.
If you have any questions or topic suggestions, please send them our way, and we will try to incorporate your request.
Please take a look at the disclaimers (https://cancersurvivormd.org/disclaimers). Words can hurt—if you feel you might get or have been triggered, please stop listening and seek support.
CancerSurvivorMD®
Survivor Chat with Brad and Josie: What Brings Us Here
Brad and Josie describe a summary of their significant and chronic health issues, which we will discuss in more detail in future episodes.
General Links:
- Disclaimers: https://cancersurvivormd.org/disclaimers/
- Brad Buchanan: https://linktr.ee/bradthechimera
- G [Josie] van Londen: https://linktr.ee/cancersurvivormd
- CancerBridges: https://cancerbridges.org/
Hello, it is April 2nd 2024. In this particular episode, brad and I will give you a bird's eye overview of some of the multiple health issues and diagnoses and treatments we've been through, and we will expand on each one of these parts of our journey in future episodes.
Brad Buchanan:Hi, I'm Brad Buchanan and I'm a former English professor. Spend on each one of these parts of her journey in future episodes. Hi, I'm Brad Buchanan and I'm a former English professor, now retired. I have had two different types of blood cancer. One was a T-cell lymphoma not otherwise specified. That took a long time to diagnose and it puzzled the doctors as to whether they needed to treat it or not. The second was a B-cell lymphoma brought on by the Epstein-Barr virus after my stem cell transplant, and the transplant itself left me pretty debilitated.
Brad Buchanan:I had an acute case of graft-versus-host disease, which means in essence essence that my new immune system started attacking the rest of my body after it had been engrafted. In me, that's the graft part and the rest of my body was the host part. So what did that mean? It meant that I had pretty awful eye pain and gut pain which turned into full-blown blindness for me. I had an unusually bad case of ocular graft versus host disease within a couple of weeks of getting my new immune system, and I also had really bad gastrointestinal GVHD, which meant seemingly endless bouts of diarrhea, long nights spent sitting on the commode because why get off the commode when I would just have to get back on it and so on. That all went down in 2016. I was diagnosed in 2015, but then they gave me some chemotherapy and some radiation prior to my transplant and I've been recovering from all that ever since. I've since recovered my vision one in each eye and then surgery for cataracts one in each eye so my vision is the least of my worries now.
Brad Buchanan:But I still have chronic graft versus host disease and I manage those symptoms as best I can. But I'm technically and practically disabled in a lot of ways. I can't run, can't play sports, can't walk long distances without feeling extremely tired. I wouldn't say I have chronic fatigue anymore, but I certainly did for a long time. But I have no stamina whatsoever. I get tired extremely easily. Walking up a flight of stairs is pretty tiring for me. It was pretty tiring for me and although I'm not considered severely immunocompromised anymore, I stopped taking prednisone just before the pandemic, which was good timing, since I could get the vaccines for the COVID-19 virus when they became available and I've had the proper antibody responses to those vaccines.
Brad Buchanan:I've since been revaccinated entirely after my transplant and so I'm not taking Pregnizor anymore, but I still do take an immunosuppressant medication called tacrolimus in small quantities called tacrolimus in small quantities, but it's remarkable how a slight change in the tacrolimus dosage has a big impact on my body still. So I still take a lot of meds and I still have medical issues that result from cancer and also from the many treatments from cancer that I've had. So I've had to retire, as I say, from my teaching job, but I try to stay busy these days by writing. I write a lot about my medical misadventures, as I like to call them, but I also write other things fiction. I write academic articles on literary topics. I just finished and published a book on Hamlet by Shakespeare, which was fun. I also facilitate a lot of online writing as healing workshops, because I've done enough research and I know experientially from my own life that writing is a fantastic way to access the emotions that lead to healing.
Brad Buchanan:Because for a long time as a cancer patient, I had to shut down my fears and go in to the treatments with my game face on, as they say in sports. I had to become a little bit of a cancer warrior. And because the language that was being used to describe my treatments was very violent, my oncologist opted for the most aggressive form of chemotherapy. When I I walked into the ER with a burst tumor in my left lung that the x-rays hadn't detected and fortunately I had my diagnosis at that point I could say I have lymphoma. Maybe you should think about that before you treat me. But yeah, it took a long time for them to figure out what was going on because they had missed the tumor in my lung. They thought my lymphoma was just along the surface of my body, along my jawline and on my abdomen. There were obvious lymph nodes that were inflamed, but they didn't realize that there was a cancerous tumor in one of my lungs. I was called at various points a zebra. In other words, my initial cancer was rare and unusual. It presented in very rare and unusual ways. And then I had an unusually difficult experience after the stem cell transplant Because they were not expecting me to have such an acute case of graft versus host disease.
Brad Buchanan:My brother was my donor. He was the golden standard for donors. In fact a younger male sibling is considered the best optimal donor. At least he was when we had him tested and he was a 10 out of 10 genetic match. And yet I still got stage four acute graft-resonance disease reaction, and for a while I wasn't even expected to survive. I didn't know that at the time, but my loved ones were basically told yeah, he's probably not going to make it at this point.
Brad Buchanan:Fortunately, that and a few other dire prognoses were proven wrong. They eventually tried a treatment called ECP or extracorporeal photophoresis. It essentially blunted the violence of the attack on my body from my immune system. I've had more than a hundred treatments of ECP over the last few years and I finally decided to discontinue those treatments and have my port line removed because my GVHD symptoms graft-versus-hostility symptoms are so manageable that I wasn't even sure that the ECP was doing any good for me any longer.
Brad Buchanan:But yeah, my life has been pretty much turned upside down by my medical problems. My marriage lasted for quite a while afterwards but eventually we split of mutual accord. But I do believe my illness, extended illness illnesses and long recovery periods and disability had a pretty tough effect. I do think that writing and talking about our experiences as former or current cancer patients or patients with chronic illnesses or even degenerative illnesses can help us cope with them day to day. And that's all we can do really is cope day to day, day to day, and that's all we can do really is cope day to day. So I appreciate you giving me the chance, dr Josie, to talk with you on this podcast and hopefully to help other people as they listen and compare their experiences, contrast their experiences with ours.
G van Londen:That's a lot of information. It's overwhelming. You experienced a lot in a very short period of time, very traumatizing, a lot of changes in your life. Your life has been turned upside down. My cancer story started in the early 2000s when I developed recurrent pre-cancerous lesions in my gynecological tract. That required multiple surgeries where they continued to chop and chop and chop away pre-cancerous lesions until about eight years ago an invasive cancer slipped through. The margins were positive and they had to add radiation therapy into the mix. Ever since then I've been in remission mix. Ever since then I've been in remission. However, in the meantime I had become postmenopausal and I was not able to have any children anymore.
G van Londen:My precancerous and cancerous lesion was driven by human papillomavirus, which is HPV. Almost everyone who is sexually active will get a short-lasting episode of an infection with this particular virus, and only in a very small population of everybody who gets HPV infection will this result in problems which we can expand on in another episode. There are some risk factors for HPV resulting in cancerous lesions. Some risk factors are known, some are not known. Some are modifiable, some are not modifiable. There's a lot of stigma in HPV which we can also talk about in the future, but I did not have any of the risk factors, and over the years I had asked multiple times why I kept being positive for HPV, which then, in my case, resulted in these recurrent precancers and eventually a cancerous lesion, despite close monitoring. And I had seen several immunologists. But it wasn't until the last immunologist, who did more detailed testing of my immune system not just the levels of my white blood cells but also dynamic testing of my functionality of my white blood cells that they discovered that I have a primary immune deficiency which I have had for probably my whole, if not most, of my life, because I was prone to getting all kinds of infections. And so I've been started since then on weekly infusions with immunoglobulins and since I'm on that treatment I have been HPV negative, which I'm very grateful for. Obviously, I'm wondering what if this had been diagnosed earlier? Could I have been spared all these multiple procedures and treatments? Also something we can talk about in future episodes.
G van Londen:And now I will tell you about my most latest diagnosis. Every time I underwent a cancer treatment or an intervention and I underwent sedation and so forth, I noticed I had a decline of my bodily function. I was able to move less, I had less stamina, and we always contributed that to these treatments. However, when I developed a pretty bad case of COVID, my stamina had totally decreased. Initially they thought I had post-COVID syndrome, but I really declined from a cane to a scooter, to a power chair, and I will spare you, in this particular episode, the details of my diagnostic route. But eventually I was diagnosed with primary mitochondrial disease. I had the corresponding genetic mutations and COVID seems to have accelerated my course. In hindsight this explains a lot, but obviously that also really turned my life upside down, because now I have a degenerative disease that's incurable and I am not working anymore as a medical oncologist. I'm fully disabled.
G van Londen:Going on disability is a journey of its own, and so, just like Brad, my life has been totally turned upside down.
G van Londen:I've experienced a lot from the patient's end how it is to navigate all of this. As a physician, I'm used to listening to others, and so it's somewhat hard for me to put all my experiences, feelings and thoughts into words in this case spoken words, which is maybe a good exercise for me. It's also cathartic, for both Brad and me. I think this will be a healing experience as well to be able to talk with each other out loud about everything that we've been through. Obviously, we have only told you a small part of all our experiences, but we will go into details of each part of our journey in future episodes and I am hopeful that you will find this podcast show or series helpful for you to be able to relate to Brad and my own journey and hopefully it will allow you to feel validated and it will allow you to feel empowered to continue to ask questions and continue to help yourself. So stay tuned for the next episode and big hugs to all of you. Be kind to yourself.

