The Q&A Files
The Q&A Files drops A Wellness Explosion
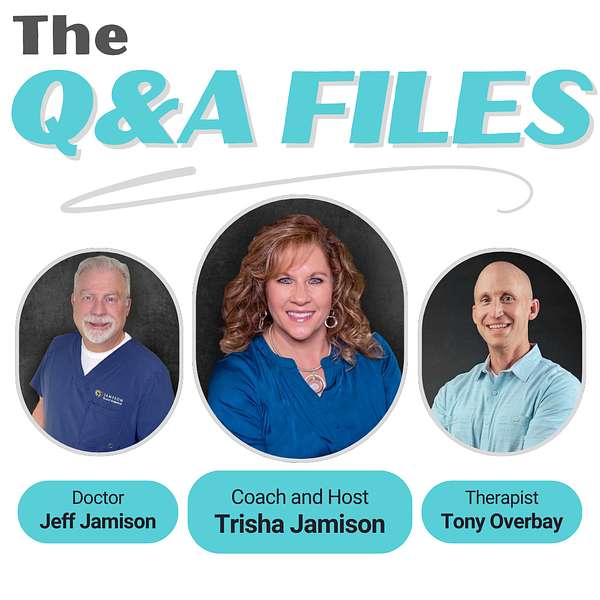
💥 BOOM! Attention Wellness Warriors. The game changer you have been waiting for is finally here. Say hello to “The Q&A Files,” where wellness meets revolution and your questions lead to new discoveries. Spearheaded by Trisha Jamison, your host, a Board Certified Functional Nutritionist. Cohost Dr. Jeff Jamison, a Board Certified Family Physician, and featured guest, Tony Overbay, a Licensed Marriage and Family Therapist. This podcast blends three diverse perspectives to tackle your questions on health, nutrition, medicine, mental wellness, and relationships. Dive into a world of expert insights and actionable advice, all sparked by your curiosity. Tune in, ignite your wellness journey, and join the Wellness Warrior community.
The Q&A Files
47. The Emotional Cost of Being Unheard in Healthcare. Katie's Cancer Story, Part 1.
Merry Christmas Everyone! Welcome back to the Q&A files.
What happens when your body is telling a different story than the medical books? Our guest Katie shares her courageous story of fighting for her thyroid cancer diagnosis, a battle she began in her late 20s when her symptoms were wrongly attributed to anxiety. Her journey is a testament to the power of self-advocacy amid a medical system that too often dismisses patient intuition. We delve into the immense emotional toll this took on her, particularly in her relationships, as she navigated the feeling of being unheard by both healthcare professionals and her own spouse.
Katie also opens up about the unique challenges of dealing with medullary thyroid cancer—a condition often misunderstood and trivialized as the "good cancer." She provides an unfiltered look at the financial and emotional strain that comes with seeking specialized treatment far from home, particularly at MD Anderson in Texas. Through Katie’s narrative, we unpack the significance of online communities and family support, illustrating the importance of finding the right medical team after years of misdiagnosis. Her story is not just about survival but about resilience, community, and the vital importance of empathy and listening for providers in healthcare.
Hello and welcome to the Q&A file, the ultimate health and wellness playground. I'm your host, tricia Jamieson, a board-certified functional nutritionist and lifestyle practitioner, ready to lead you through a world of health discoveries. Here we dive into a tapestry of disease prevention, to nutrition, exercise, mental health and building strong relationships, all spiced with diverse perspectives. It's not just a podcast, it's a celebration of health, packed with insights and a twist of fun. Welcome aboard the Q&A Files, where your questions ignite our vibrant discussions and lead to a brighter you. Welcome back to the Q&A Files. I'm Tricia Jamieson, your host, a functional nutritionist and lifestyle practitioner, and, as always, I have my wonderful co-host with me today, dr Jeff Jamieson.
Speaker 2:Hi everybody.
Speaker 1:Who's a board-certified family physician, and I'm so glad to have him here. So we have an incredible episode for you today. We're joined by Katie, and she is one of Jeff's patients and she has faced intense and overlooked battle with thyroid cancer. So Katie's story is about resilience, self-advocacy and navigating the medical system when it feels like no one is listening. So thank you, katie, for joining us today and sharing your journey with our listeners. So thank you, katie, for joining us today and sharing your journey with our listeners. Hi, so I know she's a little nervous, but she's going to just be absolutely amazing. So we're so excited, all right. So, katie, let's take it back to the very beginning. You started experiencing symptoms in your late 20s and you were initially told these were just signs of anxiety. Can you tell us what those symptoms were and how that affected you mentally, being dismissed so early on?
Speaker 3:Yeah, so I started having little like feeling like something kind of in your neck when you try to swallow and you could still swallow, but just feeling like something was caught. Try to swallow and you could still swallow, but just feeling like something was caught, like something was there, and just a little some pain in that area. And so you kind of I mean you do get anxiety from feeling something's wrong, but that just feeling that wouldn't go away, I couldn't drink anything to help it and it just the pain kind of felt like a little bit of fire going on in my neck. So I went in to seek help about that.
Speaker 1:Oh, I bet that was really terrifying. Especially you can't swallow and you know something's wrong and you don't know exactly what that's going to lead to. So, as someone going through these symptoms and not being believed, what impact did that have on your trust in the medical system and how did that affect on your trust in the medical system and how did that affect your relationships, especially with your spouse?
Speaker 2:When, keeping that question in mind, tell us what you tried to convey to the providers of care that you were talking to and then why you felt that you weren't heard.
Speaker 3:Okay. So when my symptoms progressed it was evening and nighttime, so I headed to the ER not to my normal doctor's appointment, because I felt it was emergent because the feelings intensified in my neck and I was met with when you're checking in and people looking at you like, well, your neck looks fine, you can talk, okay, nothing's caught. So then you wait for hours and then a doctor comes in and kind of looks at you and tells you that this is just anxiety. They can tell it's just anxiety and that you know nothing's wrong and you can feel something's wrong and you kind of just feel like and you can feel something's wrong and you kind of just feel like what am I feeling? Then? There's no answers.
Speaker 2:It's just anxiety, so you felt really brushed off at that point.
Speaker 3:Yeah, and they gave me anxiety medication and told me to see my family physician for follow-up. So I took anxiety medications and it did not get better.
Speaker 1:Yeah, bad wow.
Speaker 2:And sometimes it's. I mean, I can't even imagine what it would be like to be an ER physician, but you do get kind of jaded. And when you do get jaded and if a person otherwise looks like they're not going to die or they're not going to die, then in the time that they're in the ER I imagine what a lot of those docs feel is okay, they're not going to die. Then in the time that they're in the ER I imagine what a lot of those docs feel is okay, they're not going to die, they're not going to die in my watch we can go find they can go get some other care and everything will be fine and I'm comfortable shooting them out. But that doesn't mean that the person felt cared for at all.
Speaker 1:Exactly yeah, exactly yeah. Okay, now I want you to just kind of share how did that affect your relationship with your spouse?
Speaker 3:Well, early on, when it first started happening, it was just well. The doctor said this. The doctor said it was anxiety. You just take some deep breaths. It was just kind of like the focus on what the doctor said this the doctor said it was anxiety that you know. You just take some deep breaths. It was just kind of like the focus on what the doctor said and not what I was experiencing. And so not feeling like you're able to have communication and trust with someone that you know you're close to, and just feeling like you're not believed by anybody, that something's going wrong. That's got to be incredibly isolating.
Speaker 1:Yeah, absolutely Okay. So you went in, you had this experience with your healthcare provider.
Speaker 2:You weren't believed the ER.
Speaker 1:The ER you now are put on anxiety medication. You're trying to share with your spouse what's real, what's really going on, and he's trying to listen to more the medical personnel than potentially, what's happening with you. Is that correct? Yes, okay, so obviously that puts some strain on your relationship, right? Tell me more about that.
Speaker 3:Well, the as far as like with my marriage, the strain yes. Well, um, so that was a big strain we had. You know, obviously other things in life go on and um it just not feeling trust anymore, not feeling like you I'm believed, or feeling like people are attacking me, like in the medical community, like that's just anxiety, like brushing you off. And then it's also happening in your home. It's kind of your feelings are just all the way hurt. You just can't, you can't seem to open back up.
Speaker 1:Okay. So how did you cope with that emotional weight and the disbelief from both doctors and loved ones your spouse, I didn't really.
Speaker 3:I kept it all inside for a long time.
Speaker 1:Okay.
Speaker 2:Yeah, what did you do next?
Speaker 3:My next step I did. A week later I actually got a large swelling on the outside of my neck and I ended up. I was visiting over on the coast and I had to go to a different ER because I had a large golf ball size swelling on the outside of my neck a week after my initial ER encounter and they immediately jumped to action, did scans and then determined that it was just a goiter on the outside of my neck and that I was in no danger from swelling towards the inside, even though I could feel it when I was still swallowing that it was going out, not in swelling-wise, from the thyroid.
Speaker 2:Just to be clear, a goiter is a thyroid swelling nodule or cyst that is detectable sometimes by just feeling on the outside, and then certainly is able to be found by ultrasound or other imaging.
Speaker 1:Yeah, thank you for sharing that, dr Jameson. So continue on with your story. You know what happened after that. You found the goiter.
Speaker 3:Yep. I came back home and saw my family physician, who referred me to a surgeon to see if it was something that would need to be treated or taken out or what my next steps were. I met with the surgeon and he said that you know it was causing. You can have it and be fine, but because I was experiencing difficulty, swallowing at times and the pain in the neck, he recommended having surgery. And how long ago was this? This? This was in 2011. So it was it was like maybe four to six months from when I had the swelling to when I was able to have my first surgery.
Speaker 1:Okay, excellent Okay. So then what happened after that?
Speaker 3:I met with the surgeon. He said surgery we went in took half of my thyroid out, so I had a right side thyroidectomy. And waking up he said it looked good, Everything looked benign and that I could go home and just take thyroid meds as prescribed. I was called three days later and said I had a cancer diagnosis now and I needed to come back in and have the other side of my thyroid removed, which I did. So seven days from the original surgery had the rest removed and they diagnosed me with papillary thyroid cancer.
Speaker 1:Okay, so let's talk about that a little bit. What's the difference between you? I understand there's four different types of cancer. I don't know if you want to get into this, Dr Jeff, and share those.
Speaker 2:The really cool thing about Katie is she has done such great research and understanding about her own issues. She can explain this even better than I can.
Speaker 1:Wonderful.
Speaker 2:Okay, katie, I would love for her to talk through this, because not only is it personal for her to talk through this, because it it it. Not only is it personal for her, but it's also very educational for for people in my position that that sometimes don't know everything that we think we should.
Speaker 1:Fantastic Katie, we'd love to hear that from you.
Speaker 3:So I mean so the four types I so there's papillary, medullary and there's two other types right now I'm drawing a blank on, I can't remember their names. Papillary generally is not life-threatening. You can live through it. They can treat you. Medullary, which I have, can be life-threatening depending on how far it spreads and what different organs it goes to in your body. And then the other kinds are way more aggressive and you don't have much time once you're diagnosed with those. So with mine, if I would have been treated right early. There's different things Like if you would have been diagnosed right and taken correct steps, you can prevent spread and hopefully live longer. There's also two types of medullary. There's a genetic form and I do not have the genetic form. Thankfully I don't have to worry about my kids getting it. So it's just something that happened with me.
Speaker 2:So just to fill in just a teeny bit, you talked about the papillary, which is the most common type of thyroid cancer and usually easily treatable. There's follicular is one of the other ones. It's also a well-differentiated tumor that can be treated and cured in most cases. The two bad ones are medullary, which is what you described as the one you have, which is also known as a neuroendocrine tumor, as the one you have, which is also known as a neuroendocrine tumor, which can develop different cells and it can be inherited, or it can be not inherited, which you have, the non-inherited type. And then the worst one is called anaplastic. Anaplastic thyroid cancer is a poorly differentiated, highly dangerous tumor that can increase your chances of metastasis or spread of the disease and can be very difficult to treat and can spread rapidly and cause problems and is a poor prognosis.
Speaker 1:Wow, okay, so seven days in between you had both sides taken out, correct, right, tell us about that. Was that so painful? What were you feeling? Was your husband with you? What was going on in your life?
Speaker 3:Yeah, so I had young children also at the time. So the first surgery you do small scar. They had to go back in seven days later. So then I had a larger scar in front of my neck and the children were upset because and I didn't explain to them at that point about cancer they were young and just said that I had how old were they About 12, 9, and know they were young and just said that I had-. How old were they? About 12, nine and seven my boys Okay.
Speaker 3:So when? All yeah, so when that first started, so knowing something's wrong, but just saying I needed to have stuff removed in my neck, and my husband, you know he supported me. We both actually were smokers. Let's quit smoking, you know, we'll be able to do the eat healthy, do steps we need to do together and get through it. However, the doctors not my personal physician, but doctors that you go and see oh, you have thyroid cancer. That's the best kind of cancer to have. If you are going to have cancer, you got the right cancer to have. So, basically, belittling the fact that I had first of all cancer because they said it was the best kind and I would be fine. You know, as far as follow-up and I wouldn't have to you know I wouldn't have many changes besides my thyroid being removed.
Speaker 1:Yeah, so I was just going to talk about that. So the thyroid cancer is often called the good cancer those are the air quotes, which is a misconception, but your experience with medullary thyroid cancer shows how inaccurate that phrase can be. So how did you feel hearing people like your doctors downplay the seriousness of your condition? I mean, how impactful was that?
Speaker 3:I had a lot of anger actually no outlet and anger at the medical people that were around me and also towards my husband who again was like well, you know you're going to have all these. You know follow-up problems from cancer. Because they say, you know, if you're going to have cancer, this is a good type and same as my parents. You know everyone. I feel like everyone was trying to be positive and say well, you're fine.
Speaker 1:Yeah, but I can appreciate that yeah.
Speaker 3:Yeah, and I still had pain. But I'm like, well then, why am I having pain? Why do I still feel like something's wrong? And so I just by literally everyone in my life, felt like there was nobody who could understand or was there with me holding my hand. They did it in their own ways, I guess, and I don't want to be real hateful towards people, but you know it's not what I needed. I needed people to believe me that you know something was wrong, or even still have empathy for the fact that you know I'm going through something and even if you think it's not as bad the worst thing that you can have I still had my own kind of doom in myself you know Sure sure.
Speaker 2:It's never easy to have empathy for people when you don't know what they're experiencing. I mean, that's a hard thing for other people to know, but to be able to communicate it in a way that was understandable for them must have been incredibly difficult for you.
Speaker 3:Yes, and my insurance at the time did not allow me to seek counseling or therapy. They wouldn't pay for it.
Speaker 1:That's really frustrating.
Speaker 2:And, as I recall, you were working for a psychology outfit that will remain unnamed at this moment, but their job was psychological care for people, and yet their insurance company wouldn't allow it, which I thought was quite ironic.
Speaker 1:Right, oh, yeah, okay. So let's start from. You've had these surgeries. What I'd like to know is after years of pushing for answers, you finally received the correct diagnosis, but you still had a difficult journey ahead with repeated surgeries, right, yes, so what was it like to go through so many surgeries and what were some of the complications you faced?
Speaker 3:So when I went down to MD Anderson in Texas that's where I was able to transfer to because I have specialists for my type of cancer Immediately they said I would need to have surgery a modified radical neck. So I was cut from my ear to the front of my neck to remove lymph nodes and tissue and to get in there and see how far the cancer had spread. And so I went down, had appointments with them. They did biopsies, which insurance insisted on, even though they tested my original samples and found the medullary thyroid cancer instead of papillary. But I was able to have my first big surgery down there and it was obviously very scary but happy to know that we were going to hopefully get to, you know, get everything out. Because then, learning in my original surgeries, I should have had my lymph nodes removed around the thyroid to prevent spread and that didn't happen. So by the time I was able to get the correct surgery it had been another three years and I had spread in my neck.
Speaker 1:Wow, that's a lot. So we're going to touch on that clinic in just a moment, but before we go there, I want to ask you obviously you had a huge financial strain, yeah. So when you knew that you finally found the right treatment and you had to travel long distances and you're paying for various therapies out of pocket, can you talk about the financial toll this took on you and your family?
Speaker 3:Yeah, the flights. Hotels I was able to get for a second opinion, so I just had normal co-pays down there. Hotels I was able to get for a second opinion, so I just had normal co-pays down there. But, coming up with the money to travel, I needed a couple thousand dollars and it was hard. I had a hard time working. I was working and my husband was working, but at that point we were separated and so my family, my father, helped me. We were able to get the money together so I could go down the first time and then, once they're learning, you know, I think people were kind of like I felt bad, needing to go. I felt I was kind of made to feel like I don't really need to go here, I don't really need to spend this money to seek help, until we went there and found out everything that was wrong, and then more people were, you know, open to giving that help where it's needed.
Speaker 2:How did you find and decide to go to MD Anderson in Texas?
Speaker 3:So after my first surgeries I kept having pain in my neck and I went to an oncologist neck and I went to an oncologist in my town and was treated there for a little while and once they finally did a biopsy. I looked on Google, of course, and I looked on Facebook and found other people diagnosed with that kind of cancer and there was a group that had the same kind of cancer as me. I joined the group and I started asking questions and that's how I knew I needed to immediately get to a different hospital to get the right care to save my own life or try to, and have the right surgeries to stop the spread. And so that group kind of held my hand and I found who I needed to find to get me in the right direction.
Speaker 1:So you were on Google, you were researching all the things that you're going through and you found a community that basically pointed the way for you to go. Yes, that's incredible. Yes, yeah, so you self-advocated.
Speaker 2:You said I'm not getting. I don't think I'm getting what I need. I need to figure out how to get this better and I need to advocate for myself to find the next best direction to improve my situation. Am I correct? Yeah, and then so did you find advocacy with other people? You know people in your family, your community and other caregivers that were on track with that, or they were all giving you like oh, you don't need to do that, you don't need to go, you can get everything right here. Is that where you felt?
Speaker 3:Yes, yeah, I was told they could handle the problem here, even though I was diagnosed for three, four years. At this point, my family, well, they have oncologists everywhere. Well, why so far away? You can stay here. Me at first when I wanted to go, but I gained the support later after we went there and they met and heard why it's so important to go to a big hospital like that to have your treatment.
Speaker 1:And is that also where you had those multiple surgeries? Yes, okay, do you want to talk about that a little bit? What kind of surgeries you had, what did they have to take out? How extensive were your surgeries?
Speaker 2:So those are called a radical neck. Tell us more what that means.
Speaker 3:So that was my first big surgery in 2014. They removed lymph nodes, different tissue, muscles and I had cancer wrapped around my carotid artery, so they went in and they were able to peel it off. It hadn't gone through the blood supply, thankfully, so they took a bunch of tissue from my neck and sent it off for testing and after that I was diagnosed as stage four medullary thyroid carcinoma because of where it had spread into the lymph nodes, outside of the lymph nodes and into surrounding tissue and muscle. So they cleaned it up, sent everything off for testing and then I would go back every six months to have checkups down there. I'd had another surgery in 2016 to go in because I had, you know, you've got lymph node clusters all over in your neck and they go in and clean out what they can, what they see. But others will pop up as things are in them and they get, I guess, irritated. They grow large. They can then see them on scans. So then they'll go in and do another clean out as things arise.
Speaker 2:There are also testing that lights up ones that have cancer in it, and so along the way you had other testing to monitor enzymes and other things in your blood that would tell if there were any increases in that activity in your blood. That would tell if there were any increases in that activity, and so that was something that you monitored there and here in our town.
Speaker 3:Yes, yes, I was able to, which was important because I was able to work with my home physician to handle my regular things and pull the blood and do things that were needed by my cancer doctors that were far away.
Speaker 1:And who was your home physician at that time? Oh, Dr Jameson. Dr Jameson, Okay perfect.
Speaker 3:And I saw the extra people that I saw and actually you know I just want to say before I went down there to Texas I had to see all these different doctors and other people that you know oncology, see the surgeon and I finally couldn't do it anymore and I told Dr Jameson I can't see all these people, no one's believing me, it's too stressful on me to go, no one's helping me. And he was able to manage my care with Texas just in office and he was able to manage my care with Texas just in office and so important to me financially because I wasn't paying co-pays, all these different places everybody wanted me to go, but also feeling heard by my family physician and then only needing to go to oncology every six months down in Texas, far away from us, but having that relationship with my provider to understand I couldn't do it anymore and help me and just you're being believed.
Speaker 1:I mean, obviously you're having the surgeries and I'm sure that the nice thing about having someone that you're close to and has been following your care he knows you, yes, he knows who you are, he knows your personality and I think that that adds a lot of depth into that care as well.
Speaker 2:Yes, Well, and I'm sitting here a little uncomfortable as you're talking about me, but-.
Speaker 1:Well don't.
Speaker 2:Well, I just want to state, though, that this is the role of a primary care physician and this is the way it should be, in my opinion where you can be the central hub of a complex spinning wheel of care and would be the central place where those things can come to and make sure that things are handled well, and I think that that is the take-home message. I think what you're saying here, katie, is that making sure that you have a primary care physician if you're going through something like this, and lean on them and make sure you have a relationship that you can depend on, and having that relationship can be very valuable in the ongoing and actually speeding up of care. So anything else you want to add to that. I'm not trying to pat myself on the back here. What I am saying is that the role of a primary care physician can be very central to a complex set of problems that you've had to endure.
Speaker 3:Yeah, that's exactly what I mean, because I was ready to give up and not keep going if I couldn't be just believed and listened to and go on to the next step. I was done trying to seek my own care unless someone was willing to just listen. Going to doctor's appointments a week, every month, all the different specialty and everyone looking at you sideways because I had a misdiagnosis and you shouldn't be feeling what you're feeling or going through what you're going through. Little did they all know I was misdiagnosed and no one would listen.
Speaker 2:Well, I can tell you that during this time and when we were working through these things, katie taught me a lot. She taught me a lot about thyroid disease. She helped me kind of focus my own study and it helped me to be a better doctor and to listen to when people have real problems and to believe them, and sometimes it is just anxiety. But I think that even people that have anxiety can have bad problems and you can't just overlook them just because they have anxiety as well.
Speaker 3:Right, and all these things did give me anxiety, so I didn't know what anxiety and what you know.
Speaker 2:Yeah yeah, it's hard to know where the anxiety stops and the real problems start some days. Right, I misspoke that Anxiety is a real problem. I just overlooked that, like anxiety wasn't a real problem. It absolutely is a real problem, but there are sometimes underlying or overlying problems that are included in anxiety. So there you go.
Speaker 1:Perfect, perfectly articulated, thank you. So, katie, your journey is absolutely inspiring and there's so much more to unpack here, so thank you for sharing so much of it with us so far, to everyone listening. This is just the beginning of Katie's story, so join us next week as we dive deeper into her experience with MD Anderson, her continued battles and the powerful lessons she's learned along the way. So if any of this resonates with you, we'd love to hear your thoughts. Don't forget to tune in for part two, where Katie will continue to share her incredible story and advice on navigating the healthcare system. So thanks again for listening to the Q&A Files and we'll see you next time for part two.
Speaker 2:Thank, you, bye everybody.
Speaker 1:Thanks for tuning in to the Q&A Files, delighted to share today's gems of wisdom with you. Your questions light up our show, fueling the engaging dialogues that make our community extra special. Keep sending your questions to trishajamesoncoaching at gmailcom. Your curiosity is our compass. Please hit subscribe, spread the word and let's grow the circle of insight and community together. I'm Trisha Jameson, signing off. Stay curious, keep thriving and keep smiling, and I'll catch you on the next episode.










