The Q&A Files
The Q&A Files drops A Wellness Explosion
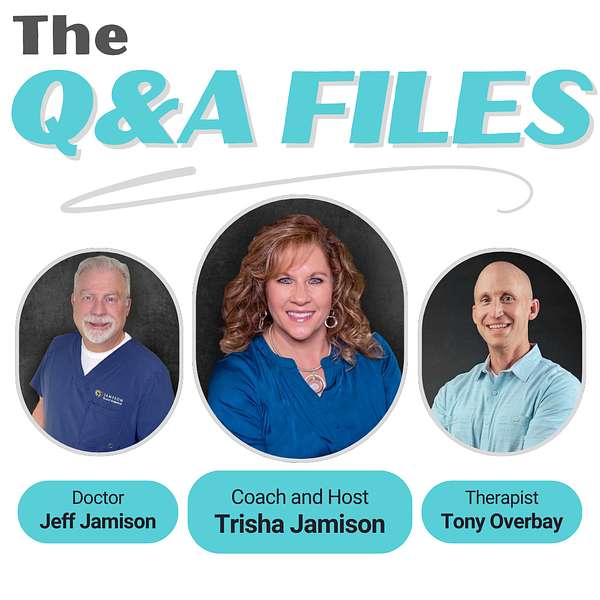
💥 BOOM! Attention Wellness Warriors. The game changer you have been waiting for is finally here. Say hello to “The Q&A Files,” where wellness meets revolution and your questions lead to new discoveries. Spearheaded by Trisha Jamison, your host, a Board Certified Functional Nutritionist. Cohost Dr. Jeff Jamison, a Board Certified Family Physician, and featured guest, Tony Overbay, a Licensed Marriage and Family Therapist. This podcast blends three diverse perspectives to tackle your questions on health, nutrition, medicine, mental wellness, and relationships. Dive into a world of expert insights and actionable advice, all sparked by your curiosity. Tune in, ignite your wellness journey, and join the Wellness Warrior community.
The Q&A Files
50. Finding Strength in Adversity: Katie's Journey Through Thyroid Cancer Part 2.
Hello and welcome to the Q&A file, the ultimate health and wellness playground. I'm your host, tricia Jamieson, a board-certified functional nutritionist and lifestyle practitioner, ready to lead you through a world of health discoveries. Here we dive into a tapestry of disease prevention, to nutrition, exercise, mental health and building strong relationships, all spiced with diverse perspectives. It's not just a podcast, it's a celebration of health, packed with insights and a twist of fun. Welcome aboard the Q&A Files, where your questions ignite our vibrant discussions and lead to a brighter you.
Speaker 1:Welcome back to the Q&A Files. I'm Tricia Jameson, joined by Dr Jeff Jameson, and we're continuing an inspirational conversation with Katie, a woman who has overcome countless obstacles in her journey with thyroid cancer. So if you missed part one, we encourage you to go back and listen. It sets the stage for everything we'll be discussing today. So Katie shared some powerful insights in our last episode, and today we're picking up right where we left off, as she tells us more about her experience at MD Anderson and how her perspective on health has evolved. So, katie, after you finally connected with MD Anderson and began receiving the right care, what were some of the biggest changes you noticed in both your treatment and in how you were being treated as a patient?
Speaker 2:Well, patient-wise, I was finally feeling believed because I was down at a place where you know they told me that, yes, this is all normal for the kind of cancer you have, and I was getting that, I had a plan and I had action that was happening and getting scheduled and appointments, and I felt like, okay, well, I'm being believed. And I felt kind of smug for a little while, like to everyone around me Like, well, you guys, something's wrong. And that also caused more problems at home because then I got more angry because I was like, see, I was right, no one believed me.
Speaker 1:Yeah, I bet yeah.
Speaker 3:That was a big challenge. How did you feel with? Sorry, I may be getting ahead of things here, but I just wondered how you felt in the community of cancer patients.
Speaker 2:So when I was diagnosed papillary which was my wrong diagnosis, everyone told me oh, that's a good cancer, you know, it's fine, no problems. And then when I had medullary thyroid cancer, which was my true diagnosis, it was well, you don't have to have chemo and you haven't lost your hair and you don't have to worry about radiation in your teeth and down the line. You know there's different treatments for medullary but at first really all they can do is keep doing surgeries. And there's other pills that you know, radiation treatments and stuff that they can do, but I'm not at that point yet. So then it became a well, I mean, it's not the kind of cancer where you have to get sick from chemo. And so then again I was well, you might have cancer, but you don't. It doesn't seem like you're ill.
Speaker 3:It's not a real cancer.
Speaker 2:Right.
Speaker 3:You didn't have to really go through the hard stuff, because if you really had an important cancer like me, then you know. Then, oh yeah, I can see how that would go.
Speaker 2:Yes, reach out for support groups or looking on Facebook or whatever. And I had to just only stick to my medullary thyroid cancer group, because if you just do a general cancer group, people kind of turn their nose up at you like, well, how dare you? You haven't been through what I've been through and you haven't been through what I've been through and you haven't been through what I've been through. But there are worse and there are better. But I could support from other people in the cancer community because mine wasn't as bad as theirs, so it was hard from all different ways.
Speaker 3:Isn't it funny how us human beings have to have some sort of competition going all the time of? Funny how us human beings have to have some sort of competition going all the time, even in dire straits. We have it worse, we have it better, we have this is a you don't know the kind of pain I've been through and we look for ways to separate ourselves rather than connect and communicate, which I think is a sad commentary on kind of humanity.
Speaker 1:Yes, yeah, definitely yeah. Thank you for sharing that. Well, I was just curious how were you feeling at that time? What were your symptoms? What was going on with you as far as just? Were you really tired? What were you struggling with?
Speaker 2:Yeah, I had a lot of tiredness and brain fog, as it's called, because I had my thyroid removed and I was on thyroid replacement and for a while, after your thyroid gets removed, they play around with med levels to see what your body needs and how you respond. So you know if you're too low or too high you can have hair loss or racing heart, cold intolerance, heat intolerance, which I had all those things at different times while trying to get my meds in line. And I also had a large scar from my ear down through the front of my which I was keloiding, so I'd have to get injections into the scar.
Speaker 2:Oh, I bet that was painful, that steroid injections or I don't know what it was, but yeah, to help stop the growth of the scar because it tightens up your skin and neck. So just physically, you know it was those kinds of things that I was dealing with. And then you know neck soreness. I had some tissue taken that side. My shoulder was tight. So some therapies and lymphatic drainage. I had to learn how to do because my lymph nodes weren't removing fluids as they needed to. So you have to learn different things with follow-up.
Speaker 3:It seems like you also had some GI complaints with that as well at that time.
Speaker 2:Yes, I did. I had a lot of problems Needing the bathroom, finding out where a toilet was, all over my town, anywhere I go, a lot of problems and I still in my neck the pain from just the muscles being tight, the surgery sites, all of that.
Speaker 1:So how long did things take to settle down?
Speaker 2:So, from physically, I had my first big surgery in 2014. It kind of starts settling down after a year and then in 2016, I had to go in and clean it out. Do it again Takes about a year. Well then, 2021, I had another surgery and I had my recurrent laryngeal nerve.
Speaker 2:Yeah. So I had cancer wrapped around that and they thought they could peel it off this time. They couldn't, so they had to cut it on both sides and they, you know, fused it back together and tested it and before they closed me up they thought everything was working. But I did end up with a paralyzed vocal cord and so I had to do speech therapy and then I had a lot of nerve pain after this last surgery and so it's been three years but I still have problems with my speech.
Speaker 2:I have like if I eat a salad I'll choke on lettuce because things don't function right inside my throat now. So I constant follow up with speech and again back to feeling like there's something there that I'm going to choke on all the time in my throat. So that's, it's just. It's never ending. You still, you learn to manage the symptoms and the problems that come from it and it just takes, you know, finding the right providers, I guess, to help you through it. I found a therapist and she was able. I did have a whisper voice, I wasn't able to project at all, and working with her I'm almost back to where my voice was before surgery and my vocal cord is still paralyzed. So are you in any kind of therapy right now? I was finally able after I got on just my husband's insurance I was able to start therapy meant for my mental health.
Speaker 2:So for the past couple of years I've weekly in mental health therapy and that's the only therapy I'm doing right now has it been helpful for you yeah, it's um, I had been having emdr and it's nice and they kind of force you to unpack and yeah, they do it's hard, yeah, it's so good, though it drains you and you're tired and you get like man, I feel like, feel like I'm sick, you know, for a day or two after. But I didn't used to be able to sit here and have a conversation about my cancer history without falling apart or just not talking. It was too hard. Now I can.
Speaker 1:Well, excellent. Yeah, that letting go thing is really powerful. Yeah, yeah, very good.
Speaker 3:It really puts your body on flush, though, doesn't it? I mean it tears, and it creates the kidneys to really kick in, and so, you know, urine is just a heavy flow for at least eight to 24 hours after EMDR. For at least eight to 24 hours after EMDR. And, by the way, it's a rapid eye movement therapy that is especially good in helping people heal from traumatic events.
Speaker 1:So that's what EMDR is Age for trauma, excellent. So looking back, katie, is there anything you wish you had known earlier in your journey that might have changed how you approached your diagnosis or care?
Speaker 2:Looking back. Well, you know I at that time I had young children. I wish someone would have told me to get my children I'm going to get teary now to get my children in therapy. I was really when they finally found out what was going on and I was struggling. I ended up getting a divorce and so my children were kind of in an upheaval of their own lives and I wish I would have tried to work full time. My kids in school deal with my personal health. I wasn't able to get my own kind of counseling when I was first going through all of this and by the time I was able to get a grasp on it for myself, my children were.
Speaker 2:I had a couple of children who one especially took a wrong path and kind of had a real hard time in his life, bad choices, and it was hard because I needed therapy for that too, because my son was rejecting me, didn't want to be around. It was hard for him to even look at me with my huge scar and the things that were going on at home. He didn't want to face it himself. How old was he at that time? He was 12 when it started and when he became 14,. 15 is when we really had a lot of family dysfunction going on, because that's when my divorce happened and my major surgeries. When I had the first major surgery, we kind of had to sit down and tell the kids what was going on, because once you hear you're stage four, you don't want to just, you don't know what's going to happen. So you kind of have to just be honest, like and tell them. And so we did, and that kind of I wish I would have been able to tell them in therapy with help.
Speaker 2:So, that's something to look back on. And also my husband we did get a divorce and I guess now I can look at it like if the doctor is telling me you know, nothing's wrong with your spouse and your spouse is saying something's wrong. It's kind of like they're caught in the middle too, you know, and so I'm able to have empathy for him. And what happened then? And I wasn't able to back then. I wasn't able to look back anywhere but myself.
Speaker 1:Well, you're in crisis, yeah, so you're in that survival mode for sure. So what happened with him?
Speaker 2:We got a divorce. We stayed living together because we got the divorce and we hadn't moved separate from each other yet because we were waiting financially to. We were only renting at the time. So we were waiting. And then I got the call that it was stage four and he said, well, I'm not going to move out. And I said okay, and he's like we'll just figure out getting through this. And so we ended up reconnecting and we were able to him coming with me down to Texas to hear from those doctors and hear I probably helped him here. You know, your wife's not crazy and just making things up and I was able to look at it from another perspective as well. So we actually got remarried.
Speaker 1:Wow, that's awesome.
Speaker 2:Yeah, it's a happy story in the end, but in between there was a lot of.
Speaker 1:Oh my gosh, I can't even imagine. Wow, that is a really hard story. But just like you said, what a happy ending. I mean you're still going through it, of course, but I mean you've got the support that. Yeah, that's a great part of that. I love that.
Speaker 3:But you also know, I think one of the things that's important when it comes to these kind of relationships, when people are in crisis, that if you can figure out a way to maneuver through it, you will grow stronger together. Because of those things. It's kind of like going to war together with a person. They're going to be somebody that, because you went to war with them, or you went through this strife with them, that all of a sudden you become closer and you can relate better to each other because of the experience. Would you find that to be something that helped you, katie?
Speaker 2:Going through the experience together. Yes, I think it kind of it helped him as well. I mean learning more about and we were young and you know it's been years now and learning how each other handles crisis as well and how different people react. But, yeah, coming out stronger, because we did go through all of that together and now, when something's up and something's wrong, I'm able to clearly say, hey, well, I know something's wrong and it's okay, and I have no fight about our finances and continuing to go to Texas for my follow-up care, because it does put a strain on our finances, but it's necessary and we both know and believe that it's necessary now. So you know it's.
Speaker 3:So you feel more prepared.
Speaker 1:Yes, well, and you've got that support that you didn't have before, so that's got to be so. You know such a different feeling now that you didn't have before. Yeah, yeah, okay, great. So, with all that you've gone through, how have these experiences changed your perspective on health and your wellbeing, and what does it mean to you now to have a healthy life?
Speaker 2:Well, I mean my experience on health. Well, I feel like we should all strive to be healthy, but the healthcare field you have to there's a saying in my medullary cancer group is you got to drive your own bus and you have to really be clear. And if you're with a doctor and you're seeing somebody and they're not standing up to your expectations or listening, it's okay to say they're not standing up to your expectations or listening. It's okay to say we're not a good fit and I need to find someone else who is, and it's okay. And I don't mean like just go around and doctor shop, but if you're somewhere and you're trying to work and get healthcare and you're not being believed, it's okay to ask for a second opinion and it's okay to take a step back and go somewhere else if you feel like you're not being treated correctly. And I wasn't able to stand up for myself in the early days.
Speaker 3:That is clearly not the problem anymore for you.
Speaker 1:Well, you don't know what you don't know, you know Right.
Speaker 3:And it's been really fun for me to be a part of this process because I've been able to see the growth that's happened with Katie and to be able to see her go from somebody who, just you know, basically took whatever a person said as base value and moved from there to someone who comes with an agenda to an appointment. She's prepared when she comes. If she needs a certain paperwork filled out, she's got most of it done beforehand. You know there are things like that, that if you are really trying to maximize the time with your physician or whatever caregiver that you're working with, I think there's a whole bunch of things that Katie does that has helped her gain her direction and to be able to get where she wants to go. How do you feel like you have changed yourself to be able to be prepared for those appointments?
Speaker 2:Great question. So I would show up to appointments, just looking at you know, like waiting for them to tell me Hmm, Great question, going to do this scan or anything else, and nothing gets accomplished and you feel like nothing's accomplished. So I feel like when you're going in, I'll have done research, or if something's going wrong, if you go in saying, and with any form of health, not just with my cancer like hey, I'm having these pains and I'd like to get my gallbladder. A gallbladder scan Turns out I needed it and you know. So things like that, like here's my symptoms, here's my symptoms. I'd like to know if we could do some tests, or I'd like to know this clearly stated what's going on, what's going wrong with you?
Speaker 3:And then being proactive about it, yes, and say, ok, let's, what are the options, what's going wrong with you? And then being proactive about it, yes, and saying, okay, what are the options, what can we do? To work on this and having some ideas in your mind already of what you're thinking. That has helped me. Like I've said before, katie has taught me so much about how to be a better doctor by her personal study about herself and for me to be able to follow up on the things that she said.
Speaker 3:The other thing that develops as you work through these things as a physician, for me is the ongoing development of trust, and when you can trust a person, you don't immediately think, oh, it's just anxiety, it's all in their head, and I'm sure that people feel like that a lot with their caregivers or their providers, and that's something that I never want anybody to feel like when they come to see me, but it still can happen. So, having that trust though develop because you've done your job and helped me do mine, it is incalculable how much it improves those contacts.
Speaker 1:Yes, so so good. We have a daughter that has had some very challenging diagnoses and we have found ourselves in your position and not knowing exactly how to help her, what to do, and she just has a myriad of so much going on with her, and sometimes I don't think she is believed by physicians either, and so it it has been.
Speaker 3:Really, it is really hard, it's frustrating, and I think that sometimes physicians, when a person comes in with varied and a lot of different issues, that the physician or nurse practitioner or whomever they get overwhelmed. You get overwhelmed. You've got so many pressures. You don't know what the pressures are of the provider that's coming in to sit down with you. You don't know how many patients are behind you. You don't know how many patients that is, somebody else waiting in the room next to you. That is really upset.
Speaker 3:You may have just come from telling somebody that they had new cancer and then you've got to go see a new baby or there's all kinds of different stressors that happen on the provider themselves. So when you're prepared to go into an encounter with a provider a doctor, nurse practitioner, PA, whatever making sure that you know what's going on with you and be able to articulate that ahead of time, and sometimes that writing it down, having specific questions, and then sometimes even giving those questions to the person who comes in so they can look them over ahead of time, Because if you've got 10 things down, very likely two or three of them all relate to each other and you can kind of clump them together and make them all go away quickly. And that's one of the things that I've learned from Katie is that she comes prepared. It's like we had an appointment just recently and there were things that she was concerned about, and I think that we communicated well. What do you think, Kate?
Speaker 2:Yes, we definitely do. You know, I have a symptom of something. These are the things I looked up and I would like to know if we could test that. And yeah, it's very smooth.
Speaker 2:And my early appointments were like well, I have diarrhea, my neck hurts, I'm having nausea, you know all over the place and before you know what's going wrong, and you're coming in with 27 symptoms, all of it side effects from my cancer and the numbers being thrown off into my blood. But at that point we didn't know what was wrong. So everything I'm disorganized, I go into an appointment, something's wrong, all these things are happening. That's something I've learned is I can't expect that one provider is going to be able to just snap their fingers also and know what's wrong with me. It does take time and so having empathy for the patient, but also being able to look at the provider and say it's okay to not know what's wrong, but can we work together to fix it? And being able to trust that that provider is going to listen and take you along and let's figure it out.
Speaker 1:So what's a key tip that you can leave with listeners with what you just said?
Speaker 2:Just being upfront, honest about what you're looking for out of your appointment. Okay, writing things down. Yes, yeah. Excellent and being ready and organized.
Speaker 3:Huge help. I can't tell you how many people come into my office and say, well, I need this paperwork or that paperwork, and then they don't bring it, yeah, and and it's like, uh, well, um, how am I supposed to do that? Because you know what they don't, what they figure, what some people figure and I know you don't, katie, because you're you and I've been working together a long time but what they figure is that, oh well, I'll bring it in a couple of days, you can get it done and back to me in a half hour, like you have nothing else to do but whatever they need you to do. And so, having those things prepared and be ready at the time of the appointment, chances are you're going to get them taken care of and be done with at the time of the appointment.
Speaker 1:Yes, well, and I really like this because I think so often we forget what the physician has on his plate her plate and so, just like Katie, she's being very respectful of his time by making sure that she is prepared, she's got things written down, she's looked up things to ask the most pertinent questions. So I think that those are really key things to really think about and focus on.
Speaker 3:And I think some doctors are intimidated by patients that do their own research. Oh, I looked up on Google and this is what I found. Don't let that discourage you anybody from doing your own research After Google, Because sometimes the Google things are great and sometimes they're not, but you can easily sort through those things when you sit down together. But don't let it keep you from doing that. And don't let the ego of the provider discourage you from doing your own thinking. That's okay.
Speaker 2:Yes.
Speaker 1:Excellent. So, katie, what motivates you now to keep going, especially on those tougher days?
Speaker 2:Well, after getting remarried my husband, I just love this story.
Speaker 2:This is a true love story we had a daughter and she just turned five, so that gets me out of bed. And when I was in the depths of all of this I got a couple of cats. Actually and not really I had to get up and take care of my cats. I got myself something. You know my boys, they'd be at school, but at first I was just I need something that you know cats will love you and not talk back to you. So it kind of helped me being able to do something all day long, and the kids as well, to kind of focus everyone's attention, and so that really kind of helped us. But as far as now, I'm in a better place with my marriage. I'm in a better place with my kids. I mean, everyone's grown up a little bit and just ask that question, yeah.
Speaker 1:So good.
Speaker 3:And thank you for letting me be a part of this journey with you. I've thoroughly enjoyed it, even though times have been difficult for you, especially as we've gone through it. But wow, what a great experience for me as your physician to be able to walk this path with you and to be able to support you in ways that I could. But I'm also sad when I can't fix everything immediately who doesn't want to do that? But you've just always been gracious and I appreciate that.
Speaker 1:Thank you. You guys seem like you're a really great team.
Speaker 3:We have been a great team.
Speaker 1:Fabulous, great. So, katie, did you have you guys had family counseling? Were you able to get that extra support?
Speaker 2:I just took myself. Insurance doesn't pay for family or marital counseling, so I just started taking myself to therapy and working through what I needed to work through. And something important that my therapist told me is I have to work on myself separate, and so my husband would need to work on his self. But you can't just throw two people into a marriage counseling and think things are going to get better. You have to do the work individually as well. So that's what I'm working on personally is just my weekly sessions with my therapist and working through my own feelings and emotions of everything and going forward. Yeah, excellent, that's awesome.
Speaker 1:And lots going forward. Yeah, excellent and lots of hugs. Thanks. So, as a last question, katie, what message would you like to leave our listeners with, especially anyone who might be in a similar place, feeling dismissed or lost in their health journey? Keep?
Speaker 2:asking questions. I just kind of laid down and let them make decisions, like I had things I didn't need to have happen to me, like radioactive iodine that I never needed because that cancer. Them telling me I had a certain kind of cancer and treating it with certain things wasn't right. And I felt like it wasn't right, but I just did it anyways because that's what they told me to do. So always it's okay to ask for second opinions and I think everyone should always get a second opinion, even if they're told by a doctor hey, this is exactly what it is. If it's something really scary like that, I recommend everyone get a second opinion and then you're able to sort through the different information that you're given Fantastic.
Speaker 1:Dr Jeff, is there anything that you would like to add?
Speaker 3:No, I think I kind of interjected as I went along and I'm entirely grateful for Katie and for the time that she spent with us and the insight that she's given. And, like I said before, I have learned so much from my association with Katie over the years and I think that we've been a good team, so that makes me happy. But at the same time, it's those kinds of trust relationships that build the best bonds and the best teamwork for getting through healthcare issues.
Speaker 2:Yep.
Speaker 1:Well, katie, we just want to thank you so much for sharing your story with us. Your resilience is absolutely inspiring and your courage to keep pushing forward is something that will resonate with, I know, so many of our listeners. So, for those of you listening, if Katie's story resonates with you, please reach out and let us know. We'd love to hear your thoughts and connect with our growing community. If you enjoyed today's episode, please consider leaving us a review and share it with your friends and family and allow us to continue growing this community of listeners who support and uplift one another. If you have any questions about health relationships, medicine or personal story you feel could help others, please don't hesitate to reach out and ask your questions. So please send them to Trisha Jamison coaching at gmailcom and we'd love to discuss your question or perhaps even have you on our show today. So thank you so much and again, thank you, katie, and we will see you next week. Bye, everybody.
Speaker 3:Bye. Thanks, Katie.
Speaker 1:Thanks for tuning into the Q&A Files, delighted to share today's gems of wisdom with you. Your questions light up our show, fueling the engaging dialogues that make our community extra special. Keep sending your questions to trishajamesoncoaching at gmailcom. Your curiosity is our compass. Please hit subscribe, spread the word and let's grow the circle of insight and community together. I'm Trisha Jameson signing off. Stay curious, keep thriving and keep smiling, and I'll catch you on the next episode.










