The Q&A Files
The Q&A Files drops A Wellness Explosion
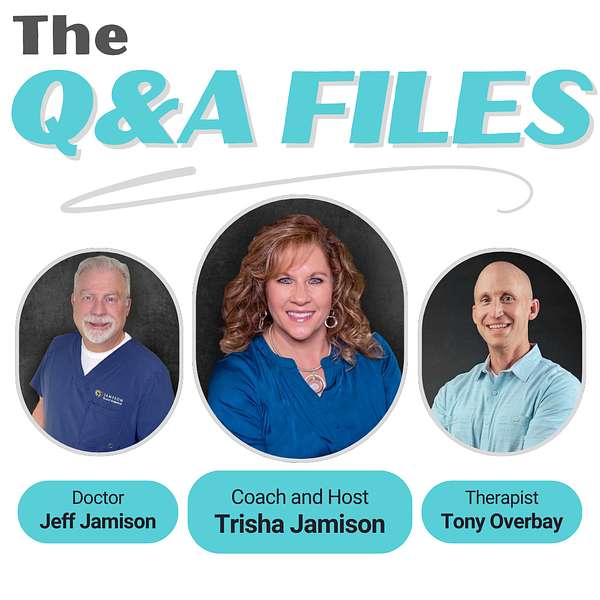
💥 BOOM! Attention Wellness Warriors. The game changer you have been waiting for is finally here. Say hello to “The Q&A Files,” where wellness meets revolution and your questions lead to new discoveries. Spearheaded by Trisha Jamison, your host, a Board Certified Functional Nutritionist. Cohost Dr. Jeff Jamison, a Board Certified Family Physician, and featured guest, Tony Overbay, a Licensed Marriage and Family Therapist. This podcast blends three diverse perspectives to tackle your questions on health, nutrition, medicine, mental wellness, and relationships. Dive into a world of expert insights and actionable advice, all sparked by your curiosity. Tune in, ignite your wellness journey, and join the Wellness Warrior community.
The Q&A Files
56. The Heart of Behavioral Health, Stories from the Front Lines with Neesha Wright, Behavioral Therapist and Trainer for Caregivers
Thank you for listening!
In this enlightening episode, we delve deep into the critical topic of behavioral health through the expertise of our special guest, Nisha Wright. As a Marriage and Family Therapist, Nisha sheds light on the interplay between mental health and the support systems surrounding individuals with developmental disabilities. Our hosts, Trisha Jamison and Dr. Jeff, navigate the conversation with warmth and understanding, addressing the common misconceptions that often cloud the field of behavioral health and emphasize the importance of empowering individuals to embrace their independence.
Listeners are treated to an engaging discussion that covers the role of caregivers—discussing not only the physical demands but also the emotional challenges that often lead to caregiver burnout. Neesha shares effective strategies for self-care that listeners can implement into their daily lives, reminding everyone that their well-being is just as important as those they care for. Through storytelling and shared experiences, the episode illustrates how understanding and empathy play key roles in fostering meaningful connections with those they care for.
Tune in for a significant discussion about how behavioral health empowers individuals and families alike, as we explore real-world strategies for navigating complexities with grace and resilience. Whether you're a caregiver, a family member, or someone interested in mental health, there's something in this episode for everyone. Don't miss the opportunity to learn, grow, and connect in our community. Remember to subscribe, share, and join us as we strive for a healthier, happier tomorrow together.
For questions or comments, please email us at trishajamisoncoaching@gmail.com.
Hello and welcome to the Q&A file, the ultimate health and wellness playground. I'm your host, tricia Jamieson, a board-certified functional nutritionist and lifestyle practitioner, ready to lead you through a world of health discoveries. Here we dive into a tapestry of disease prevention, to nutrition, exercise, mental health and building strong relationships, all spiced with diverse perspectives. It's not just a podcast, it's a celebration of health, packed with insights and a twist of fun. Welcome aboard the Q&A Files, where your questions ignite our vibrant discussions and lead to a brighter you.
Speaker 2:Welcome, friends, to another episode of the Q&A Files. I'm your host, trisha Jameson, a functional nutritionist and lifestyle practitioner and a life coach, and, as always, I'm joined by my incredible co-host, dr Jeff Jameson, a board certified family physician.
Speaker 2:And we don't have Tony here with us today, but we've got another amazing guest that we're so excited to introduce here. So glad to have you here, jeff, and I'm so excited for this episode and I think so many people are going to resonate with our guest and a listener question from Jodi that we'll share later in the episode. So this week we're diving into behavioral health, a topic that affects caregivers, families and individuals with developmental disabilities and mental health challenges. Today we have an incredible guest with us, someone who brings not only amazing expertise but also a deep passion for helping individuals and families navigate the complexities of behavioral health.
Speaker 2:Nisha Wright is a Marriage and Family Therapist, associate MFTA, with a Master's in Clinical Psychology and extensive background in clinical and counseling work. Her journey in this field began in 2012 as a substance abuse counselor at the iconic Haight-Ashbury Clinic in San Francisco, where she saw firsthand the challenges people face when dealing with mental health and behavioral struggles. Since then, nisha has worked across various roles with diverse populations, always bringing her knowledge, compassion and problem-solving skills to the table. Today, she serves as clinical coordinator for a supported living agency in Spokane, where she plays a crucial role in improving the lives of individuals with disabilities. She provides home visits, staff support, hands-on training and behavioral intervention coaching, while developing person-centered, positive behavior support plans that truly make a difference. We are beyond excited to have her here today, not just because of her expertise, but because she's also a great friend of ours. She's been both a patient of Jeff's and a client of mine, and now we get to pick her brain on this podcast.
Speaker 3:Which we're so excited about too. She's so awesome. We're glad to have Nisha with us.
Speaker 4:Thank you so much, Tricia and Dr Jeff, for inviting me. I'm super grateful for the opportunity.
Speaker 2:Yes, absolutely, we are so excited. So, nisha, one of the things that we start with and you're going to be familiar with this, and this is one of the reasons why I wanted to wait for you to be on right now and introduce you first and then do celebrations, because when we started our sessions, first thing that we would do would be celebration. So we're going to start again and I'd love to hear a celebration from you and Dr Jeff.
Speaker 3:And I'll start, okay, so it gives you a chance to think about it for a second. Okay, so my celebration is that last night I got to spend time with my sister and her husband, jill, and Drew Nelson. They're wonderful people and sometimes you just have to sit down with your people, and they recognized how incredibly helpful it was to just be ourselves and have a great time talking about family life and things. And Tricia hasn't been feeling that well, so she wasn't able to join us, but she encouraged me to be able to go and do that, and that little effort on her part is so appreciated by me. So my gratitude is to Tricia for allowing me to do something that isn't something I normally do and take care of me with an enjoyable time with them. So thank you, tricia.
Speaker 2:Absolutely. That is definitely a good one. There's something about sibling energy that you just need to be part of Yep.
Speaker 4:I would say my win is something also family-oriented. I had the opportunity to find some old recipes. So a little bit about me. On my mom's side of the family. She's Filipino and Chinese and my grandma used to cook and bake a lot. My mom always tells me that she's not much of a baker. I love baking and cooking. It's something I just love to do in my spare time. We spent some time together and I had the opportunity to find one of my grandma's old recipes for this. It's like a bun. It's like a. It's called shupao in Tagalog, but it's just a little Chinese bun and it seems to be complex. It's a steamed bun Should be easy.
Speaker 4:It was not my mom and I tried to make this recipe using my grandma's recipe failed the first time. It was just hilarious and fun to make that mistake, but our second batch turned out perfect and I'm just grateful. Like I sat with that, I was like this is a moment, like it was just like a core memory, like locked in, spending time with my mom and trying to do something. My grandma right now has Alzheimer's and so her memory of cooking is not there, so she can't teach it to us. So we had to go off of what we thought best out of a recipe.
Speaker 3:Wow that is really cool.
Speaker 2:Yeah.
Speaker 3:And isn't it something how those flavors and smells all bring back those positive memories of that time during your childhood. Isn't that just wonderful?
Speaker 4:Yes, I definitely had like my heart was like just so warm.
Speaker 3:After that I was just like, oh my gosh, it tastes in the oven and I just would love that Now, when I smell chocolate chip cookies or any cookies really in the oven, it brings me back to that wonderful time in my childhood.
Speaker 4:It's so interesting how our mind just kind of remembers that and has associations with smells and taste.
Speaker 3:Yep. It's very interesting.
Speaker 2:That's so fun.
Speaker 3:Okay, Tricia, what's yours?
Speaker 2:and taste. Yep, it's very interesting, that's so fun. Okay, tricia, what's yours? Well, I have two celebrations. First one is about Dr Jeff, because he just got off a grueling six weeks of being alone in the office. His other provider has been out on medical leave and it's been pretty rough and he got beat up pretty good but he did it.
Speaker 2:And I feel kind of bad because I was out a week with our son, chase, and that's going to be my second celebration I'm going to share. But I came home from an event and I got super sick and he kept me alive. He literally did. He placed his hand on my back one night just to make sure I was still breathing because I was so sick. But he just worried about me and I just I did feel terrible because he worries about so many people and I didn't want him to have to worry about me too. But it was so nice to have him be there and just show up like he would normally show up and I'm just so grateful for him and the knowledge that he brings because he made me all better.
Speaker 2:So that's my first celebration is I'm thanking Jeff. And then my second celebration is I got to go to Vegas and actually Jeff was the one that was supposed to go with me, but because our provider mid-level provider was unable to cover, because she had a medical issue that was really important, and so I took our son and it was phenomenal. We had so much fun. We went to a. It was basically almost a week long. It was like a rock concert for entrepreneurs and I don't know if you've ever heard of Russell Brunson or ClickFunnels or Funnel.
Speaker 3:Hacking Live yeah, Funnel.
Speaker 2:Hacking Live. He just he's this amazing, amazing marketer and got to enjoy him. And then, at the end of the week, Tony Robbins. We got to be part of that whole experience and it was crazy because he was there for four hours. I don't think anyone left the room. There's 5,000 of us and he had the whole room. There was so much energy. It was literally one of the most phenomenal experiences I probably have ever had, the most phenomenal experiences I probably have ever had, and he just shared some of the most incredible, inspiring stories and, anyway, I learned so much this whole week, came home, shared it with Jeff and anybody else I can. It was just so inspiring. So sad Jeff wasn't there Was so glad our son was able to come and he's also on our team and helping us with a lot of different things, so we're excited to have him on board.
Speaker 3:That's awesome.
Speaker 2:Okay, so before we share our listener question from Jodi, we have several questions that we would like to ask you first, nisha. All right, all right, you ready.
Speaker 4:I think so.
Speaker 2:First of all, what inspired you to pursue a career in this field and what led you to Spokane?
Speaker 4:I was born and raised in Spokane. My family Air Force, so my family were both in the Air Force and I was born at Fairchild. So I went to college at Evergreen State College in Olympia and that was my first journey for college. And then I went to college at Evergreen State College in Olympia and that was my first journey for college. And then I went to school further in San Francisco where I don't know something just came out in me I've always been a helper. I've always wanted to help my family really instilled volunteer work. At a young age People felt naturally drawn to talk to me and open up and I just I don't know it felt really natural. It didn't really I didn't really notice like the whys of it just made it was a fluid change into why I ended up in the field. I started out with substance abuse, substance abuse clinic, working as a counselor there. I did my trainee experience there. Yeah, it was just really positive.
Speaker 4:I don't know the support there at the Haydash Berry Free Clinic really was a good foundation. I loved learning. I loved just being there and finding ways to support people with different challenges. Whether it was substance abuse, it expanded into family Again. Mental health and substance use affects the whole family, so there was never a time where I'm working one-on-one with someone where the whole family isn't considered and I think I just really appreciated that. It made me reflect on my own life, my own family systems. I have had family members, extended family, who have struggled with substance use and mental health issues and I think part of that also just sparked my interest.
Speaker 2:Excellent, well, thank you. Okay, so I want to start with the bigger picture. People hear behavioral health all the time, but many don't fully understand what it encompasses. How would you define it in a way that makes sense to the average person?
Speaker 4:I would say that's a great question. I would say behavioral health just as kind of encompasses, I think, a little bit of everything our mental health, our daily, our environmental, our social I think it's an overarching word to say like everything in our social, environmental life. I'm trying to like think of that question. It's a big one. I don't know where to start because I think it's a big word to say it's a little bit of everything. Like mental health is under behavioral health. Behavioral health is just everything about how we are as a person, why we do the things we are, who we are. I'm not exactly sure how I want to even answer that.
Speaker 3:So I like to listen to this. Have you ever heard of Hitchhiker's Guide to the Galaxy? Yes, okay, and it's kind of like the answer to life, the universe and everything. Okay, and that's kind of what I look at behavioral health as like the answer to life, the universe and everything. Okay, and that's that's kind of what I look at. Behavioral health is like the answer to life, the universe and everything. It sort of encompasses everything and, by the way, if you look at the Hitchhiker's Guide, the answer to life, the universe and everything is what? Yes, it's 42.
Speaker 4:Okay, I mean that's, that's a.
Speaker 3:it's just a hilarious look at that, but I just appreciate where you're coming from and kind of struggling with that answer because there's so much. Okay, Tricia, give her an easier one next time.
Speaker 4:Yeah, I was like that was the first start and all I could think of is an onion.
Speaker 3:So I think a lot of things is an onion, I was like this is a big word and I'm peeling back, but the more I start to talk, then I'm going to keep wanting to add more to this onion and I don't even know where it's going to end up. Yeah, but that's an answer in and of itself, right there.
Speaker 2:So the end we can even, as time goes on, we can just continue to answer that question as well. So yeah, definitely. Now, in your experience, what are some of the most common misconceptions people have about behavioral health and developmental disabilities?
Speaker 4:individual with disability cannot do anything for themselves, that they need 100% support all the time, that they can't strive for more independence, and that people who provide supported living services to that individual take away all choice and power of that individual. In reality, a person who's supporting a person with a disability, they're working on helping that individual find their independence, find their power and choice, and they're more of an advocate.
Speaker 3:Oh, I love that. That's beautiful.
Speaker 4:And that's really. Yeah, I see that every day.
Speaker 4:It's like you're not allowing them to be more independent, or sometimes the stigma that a person with disability and mental health issues does not have the ability to make choices or make mistakes, that they're not in a mental capacity where they could make decisions and allow that just natural. Hey, I can make a mistake and learn from it, and reality-supported living really does allow enough space when I mean depending on situation, obviously, but does allow a space for an individual to make a choice, make a mistake, learn from it and grow.
Speaker 3:I think one of the things that I see is the opposite too. If a person is they have some mental disability, or they have some disability, whatever it is, and they want to be treated like they don't have any problems, and then sometimes people expect them to do more than they actually can. People expect them to do more than they actually can no-transcript what they can do and what they are striving to do, and helping them, helping a person reach those goals without getting in their way. That is just. That is a a challenge and a gift for those who do it.
Speaker 2:So congratulations on that yeah, I I have to agree with that, and we've we've got situations that we are dealing with too here, and it definitely is challenging because you want to be able to give them so many opportunities and then when you recognize that those are too many, but then when you have to kind of reel them in a little bit, then they get frustrated. It's like, well, how come you took that back, or but it's, they're not ready and so, yeah, it's a lot sometimes.
Speaker 3:Yeah, it's a moving target.
Speaker 4:Absolutely, and I think I give kudos to anyone who's a family caregiver or family support not doing it with the support of like agency. So I think the difference in the agency level is we have different support people, whole team. But if it's your own family member that's struggling with that disability and you're trying to help them be the best they can be, but also set up reasonable goals and help them find a place where, hey, this is what's doable. Right now I think it's even more. It can be heartbreaking. It could be just a lot to handle.
Speaker 4:So, I always give kudos to anyone who's doing it without a support network.
Speaker 2:Yeah, excellent, okay, well, thank you for that. So this question is for both you and Jeff. From a medical standpoint, I see the physical and behavioral health are closely connected. I see the physical and behavioral health are closely connected. Can you talk about why understanding both is essential for providing the best care? Jeff, you want to start? Oh, this is great Sure.
Speaker 4:I know that is a good question.
Speaker 3:Yeah, this is a great question and one that I consider in every patient encounter, because nobody shows up in an appointment or in a care situation that they don't bring the baggage with them of whatever their problems or things that are going on in their life present, and very often there is a mind-body connection between whatever that's going on with their body that they're coming to talk to me about. Usually it's something physical, a pain, something that is not properly working in their abdomen or whatever the case may be. One of the things that I try to do is decide how much is strictly physical, which sometimes it is, and also how much that their own environment and the ways that they're reacting to it is entering into the physical manifestation of their disease. Sometimes, especially when it comes to abdominal pain, bowel function, twitches in their face or eyes there's all kinds of things that really quickly manifest in a person that's under high stress, and stress can be manifested in so many different ways. You know it could be a family that the mother and father are at odds and they're not doing well and they're trying their best to hide the problems that they're having from their children, and so they're clamped down on the emotions that are going on inside them so they don't show them to their children. That can cause manifestations in so many ways. I mean, that's just one thing that comes to mind, but keeping in mind the psychosocial part helps me with the physical part.
Speaker 3:And the other thing that I think about too is sometimes I forget to get to know a person first, and that's one of my first things that I like to do when I meet a new patient is not to just say okay and launch right into what their problem is, which is the way that most doctors do. They say they look at their chart or their paper in front of them or the computer, and they're not looking. I'm holding my hand in front of my face, so the person can't really see me. And what they do is they say, oh, looks like you're here because you have back pain. Okay, and so how long have you had back pain? And they don't even know anything about what happened to this person. They just launch into their standard questions. You know my way to do this and I'm not saying that I'm the only way to do it, but this is my way to do it is to walk in the door and say, okay, hi, I'm Dr Jameson Tell me about you, but I don't want to know anything medical about you right now.
Speaker 2:I just want you to tell me who you are. I love that. There you go.
Speaker 3:Tell me about your family, tell me about your. What kind of work do you do? What kind of stress are you under, what are the things that are happening in your life that are important to you?
Speaker 3:And I take a minute or two just to understand the human being and then ask the other questions human being and then ask the other questions and usually in a new patient encounter the person is like I've never had anyone ask me that before. I don't know what to do. I don't even know what to say. They're totally deer in the headlights when I ask them that question. So I have to prompt them, say okay, tell me about your family. What kind of work do you do? Oh my gosh, you are under a lot of stress, you know, or whatever it is that we you know. So I get to know the person. And when you can get to know the person, the human being behind the problem, often the problem will reveal itself easier. And the other part is the person is disarmed about you as a physician coming in and not being a human being yourself. Dr Jeff Yep, go ahead.
Speaker 4:I was going to say. I can attest from that from my own experience too. It is slightly alarming if you're used to providers not asking you, hey, how's it going? And getting to know you and I think it's you know it does make you feel safe. I think setting up that safe space and that safe foundation you'll get to learn so much about what that person's going through, and I think what you mentioned about it being mental health and physical health go hand in hand I mean back and forth. And the only way you could kind of unpack and decide where that's coming from or what the issue is if the abdominal pain is an emotional pain is getting to know that person, and I definitely appreciate how you provide that safe space as a practitioner. It's super important and it's so crazy how different it feels when someone asks you, even starting with how are you doing? How was your day? That?
Speaker 2:was a common practice and it's really shocking for Jeff. When somebody asks him he doesn't even. He's like huh what. When somebody asks him about how are you doing, are you doing okay and shows that kind of care for him.
Speaker 3:Yeah, that's been really super the last few weeks that we've been working with no other provider but myself in the office. That's been a little bit of a challenge and my staff has been very good about letting people know you may have to wait a little longer than normal. You may have to wait a little longer than normal to get in these things, so that patients are understanding and then they do ask me and you know I'm really lucky to have patients who we care about each other more than just a okay, I'm here to get my needs met and I'm out the door kind of doctor-patient relationship. And that's one of the great gifts I think of family medicine is being able to have an ongoing relationship with people, is being able to have an ongoing relationship with people.
Speaker 2:Yeah, beautiful, I love that. Thank you both so much. Nisha, you talked about how you create behavioral support plans for individuals with disabilities. Can you walk us through the process? How do you go from assessment to an actual plan that works?
Speaker 4:Yeah, that's a good question. Most of the time it's as you know. We've been talking about already getting to know the individual. It's spending a lot of time. It's doing visits. Before I even start a plan I'm like what do they like, what do they dislike, what do they enjoy to do? For? Like the very, very basics. What do I know about their family history? What impacts them? What have they told me has impacted them day to day and makes it hard to do A, b, c, d. So getting that foundation, that's my start of writing a plan. After that it's working on a team. What have we tried? What are the behaviors going on? So there's that, identifying what's working, what's not working. The whole goal of the plan is to find proactive strategies to prevent something that's not going great and find those coping skills to throw in there and help the individual work through before it gets to something super, super negative.
Speaker 3:What are a couple of specific behaviors that you see a lot that you have to work with.
Speaker 4:Absolutely so. Right now, ones that I'm seeing a lot are property destruction just due to not getting a desired meal. So it's something it can be super simple. So, okay, they're punching a hole in the wall because they're not getting their desired food. What's really going on? So I think you know at my job we spend a lot of time in teams. Okay, what is this person trying to communicate right there? What is their need? Are they hungry? Are they just bored? Do they not like the staff they're working with? And we need to build more rapport in the home with that staff.
Speaker 4:That's a lot of again, picking the pieces and trying to learn this individual and what works and doesn't work.
Speaker 4:And once we find that kind of little like green area or that like area where they're in a calm state, we could practice and see what works with coping skills. So we're not going to jump in to take a deep breath or let's pause and do some mindfulness skills. I've already experienced we're not doing that when they're already throwing and punching things in the wall. So what we want to do is find things that work when everything is fine and then build off of that and then also just looking at the strengths Every individual I've worked with has so many strengths. I have individuals that are just really strong readers, and so they're going to read the skills to me and we're going to practice it. I'll model it, they'll model it back. All of these things are what go in the plan, and it's kind of almost like a guide and instruction for the staff who work with that individual 24 seven on how can we help them when things are getting tough, before it's at the red or at the escalation point.
Speaker 3:So it sounds like that every individual's plan is as individual as the individual.
Speaker 4:Absolutely, and that is the goal. We want it to be strength-based. We want it to be so specific that if you write it without a name on it, you know exactly who, which individual, we're talking about, down to their favorite color, their favorite food, who their support network is, who they want to talk to when things get tough.
Speaker 3:Well, that's interesting because it seems like you could translate those skills into working with anyone, really Absolutely. I mean, they may not even have a developmental or other disability, but just getting to know another human being and then using those skills to not necessarily, I mean, I wouldn't say to use it as a manipulation tool, but as a way to get to know them and to be able to improve your relationship with them, not to be a chameleon for them, but to be a person that understands that individual.
Speaker 4:It's almost like an instruction guide on how to best.
Speaker 3:How to win friends and influence people.
Speaker 2:Yeah, I love that and I really I love how you adjust when something isn't working. It's not like this is the plan and it's going to fit for everybody. You find a very specific plan that works for each individual, so go into. What kinds of things would you like to include to help with that assessment?
Speaker 4:I would say like again their strengths, behaviorally, just things they can also do like skills they've tried, that they've really succeeded in and so we can build off of that. It makes it a little bit easier to keep adding skills if we know what worked and didn't work. Instead of taking deep breaths, I'm not going to say, okay, let's start again with take more deep breaths.
Speaker 2:Yeah, let's just keep breathing. All day, the more breaths they take.
Speaker 4:Yeah, so I think you know communication style. That's huge. If someone likes more space when they're upset, we want to acknowledge and respect that space is really important. Or if they need someone to sit with them, next to them while they're in a behavior and having a hard time, but they don't want that person to talk to them. We're going to be noting that and really the only way you could get the information for those pieces is spending time with them, talking to people who spend time with them, their family and anyone in their support network. Those pieces is spending time with them, talking to people who spend time with them, their family and anyone in their support network.
Speaker 3:But one of the things that I sorry for interrupting you there, but one of the things that I recognize about you, nisha, is that you're fun, you have high energy and you're funny, okay yeah. And so I wonder how you use those strengths in communicating with and being with those people you're working with.
Speaker 4:I mean I try to stay positive as much as possible.
Speaker 2:She gets along with everyone.
Speaker 4:Not always, I try but also, you know, I have to always remind myself, like where the individuals are. They have staff 24-7. It's got to be a lonely experience to not have as many, maybe as many close friends and support. That's not paid staff. That always comes to my mind. I'm walking into their home, my interactions with them. I mean, I am a paid staff too, so I want it to feel as like hey, no, I'm actually here for you.
Speaker 3:And you're kind of there because you want to be too.
Speaker 4:And I definitely want to be there and that shapes like my mindset. I always have to remember my mindset when I'm writing a plan, when I'm visiting a client, any of those situations, and that keeps me positive. I mean, just this week, one activity, activity. I'm working with a gentleman who has been diagnosed with autism and some other developmental disabilities and one of his strengths is reading. So we have these communication like what do you see going on here? What is the behavior on this card? They're just communication cards. They have pictures going on here. What is the behavior on this card? They're just communication cards. They have pictures and you get to guess what's going on in there. And he will read the cards, tell me a story based on what their feelings are, and what I've learned from this is that he's super caring and thoughtful. Like his first instinct is to this person looks hurt. I would ask them if they need a first aid kit. Like forgetting that, like there's so much more to the person than just the diagnosis.
Speaker 2:Um sure.
Speaker 4:That always keeps me in a positive mindset and that you can have fun and joke, and I mean what. I bring my personality to the home. I I try to be positive and funny because, like, it brings the same out of them and it's, it's enjoyable.
Speaker 2:Oh.
Speaker 3:I think that that's so important. For sure, and you know just, I can just imagine you know, knowing you as we do that that you're just a breath of fresh air when you walk in the door. So I'm sure that you bring a light and a fun that many others I mean other people bring other strengths, but I can just see that as a light for you to come to a person's care in a positive way and I love that about you.
Speaker 4:Thank you. I think it's a little different in the crisis situations. Maybe it's less bubbly, more practical. But I mean, when I have the opportunity to, why not be as happy as you can be? Why not bring?
Speaker 2:some joy in that moment. Well, that energy is so important too. You know you affect the room and so if you bring in that lightness and a little bit of that fun, even though you're being very professional, you know people feel that and they just feel more at ease. So I totally can see that. Thank you so much. Okay, so you work closely with caregivers and staff. What are the biggest mistakes, you see, when people try to support someone with behavioral challenges?
Speaker 4:I would say a huge piece is not not being self-aware of how they are feeling. So when things get tough, when they're working a lot of shifts, I think sometimes caregivers or staff can really forget that they need to be mindful of, like, what their needs are, so not forgetting about their own needs. Making sure they ate lunch yes, we're providing food and we're spending time with our individuals, but did you eat your own lunch? How are you feeling when this behavior is happening? Are you feeling frustrated? It really changes the energy, as you mentioned, the energy in the room. If you're hungry, if you're frustrated from the individual on how they're talking to you, are you approaching this calmly? I see a lot of staff get frustrated and then they almost get upset with, like, the individual they're working with and really the staff are the ones that need kind of like the same skills in a behavior plan taking that pause, learning what works and doesn't work, finding your strengths. I think it's the same both ways.
Speaker 3:So you have to do your own work as a caregiver before you can actually do a good job of caregiving? Is that what you're saying?
Speaker 4:Absolutely, and I think that's for job related caregiving, but even in your own personal life caregiving, I agree 2000%.
Speaker 2:Yes, when you're feeling that stress, to be able, like you said, take that pause, separate yourself for just a moment, so you can just kind of get your wits about you once again. So, yeah, excellent.
Speaker 3:I should tell you a story that happened about 10, 15 years ago, I guess, where I let my own feelings and stuff get out of control in a patient environment when I was with a patient, in a patient environment when I was with a patient.
Speaker 3:And now I can look back on it and say, yeah, I probably behaved inappropriately, but I felt like I was justified at the time.
Speaker 3:But yeah, there was a gentleman who was seeing me for diabetes and had been seeing me for several years and the one thing I knew about him is that no matter what I tried to provide him, no matter what I said, he would always do something else and he wouldn't listen to my advice. He wouldn't do any diet controls, he barely ever took the medicine that I prescribed for him and his diabetic laboratory work proved the fact that we were not getting anywhere. So he comes into me this last day that I saw him and he told me after I tried to get him to start some insulin to get his sugars under control, gone through all the education regarding it, had people supporting him with dietary and other supports, and he said that he went to the bar and he talked to a guy at the bar who said if you drink a shot of whiskey in the morning and a shot of whiskey at night, that will take care of all your diabetic needs.
Speaker 2:Oh my gosh.
Speaker 3:And I lost it. I just said no way, and that's what he'd been doing. He actually took that advice. So instead of taking the advice of the doctor, he took the advice of some bartender that you know all I need to do this. Well, so it came down to that he didn't like having diabetes, he didn't want to have diabetes, and so he wanted to act like he didn't.
Speaker 3:And he thought if he just did these other things, that it would just take care of him and he wouldn't have to worry about it. Well, I, I right then, and there I just stopped him and I said this relationship isn't working. I don't like what you're doing. I hate that you take the advice of a bartender over your doctor. And so this will be our last visit. And I just was furious at this guy, oh wow, and I walked him out the door and I sent him a letter.
Speaker 3:Yep, he got fired and the sad part is I took care of other members of his family, and still do, but he didn't last long. He died in just a few short years after that encounter. It's because sometimes, as much as I hate to admit it, we actually do know more than some of these.
Speaker 2:Than bartenders.
Speaker 3:Than bartenders yes. And so, and sometimes when I don't know, it just hit a chord in me that I can only imagine how you, nisha, have got to keep those things in check when you absolutely know more, you absolutely have understanding of what's going on, and that the client, the patient, just doesn't know what they don't know.
Speaker 2:Well, and I think it's got to be so impressive too, when you've got a client that is reacting really poorly, maybe calling you names, throwing things, I mean you have to learn how to handle that in a way that is respectful. It's not about you, but it's all about you. I mean you feel it's being done to you. It's about the patient and just ignoring those comments. The bad behavior go back to what the things in that you've learned from the beginning and going back to those basics and just being able to keep your cool. I think that that's just got to be so impressive and it takes a toll too, I'm sure, on you.
Speaker 4:I think for me, I do more of the behind the scenes work, so I'm working with the individual less than the support staff, who are there 24 hours, and part of my role is doing the teaching and training. So the behavior plan is also almost a teaching guide for the staff on. Hey, we've spent a lot of time with this person. We know a lot about them. This is to help you really put into perspective what this person has for goals, what their behavioral concerns are and how can we best help them without making things way worse. And so I definitely agree, sometimes it is hard to put your emotions in check.
Speaker 4:For me, I find it more so when it's teaching the staff. If I'm like, hey, you guys are just sitting on your phone, this person. Of course, if I were being supported by someone and they were not engaging with me for the whole day, I would have a behavior too. It doesn't feel good to be ignored in your own home. So part of my role, yeah, is spending time with the staff and saying like, hey, can you empathize with this? What would it feel like if you were in this role? Can you practice the breathing skill with them? Is there some things? And then I try to model it in the home in hopes that they can handle these big, big situations with the skills that they have.
Speaker 2:Oh, I love that. This is a great segue into my next question. This is talking about communication, so caregivers often struggle to get through to their loved ones. What are some key communication strategies that work well for individuals with developmental disabilities?
Speaker 4:That absolutely is a good question. I think patience a huge piece is being patient and not setting an expectation that you're going to get the answer the way you want the answer, and really just honing in and sitting there with your individual, with your family member, and getting to know them. I think that is the key piece over and over again Really listen and figure out or listen what they're saying, what they need, and I think that gives you a lot of answers.
Speaker 3:How do you help a person in that situation understand the boundaries, though? I mean. You can't just let them get away with every bad behavior just because you're being patient.
Speaker 4:Oh, absolutely no.
Speaker 4:I'm being patient with the listening to learn about what their needs are. I think being comfortable and practicing, setting healthy boundaries are the boundaries that need to be set. I think it's hard to answer without, like, a specific scenario in mind. But yeah, I think the self-care is going to get you a long way as a caregiver, a family member, being open to listening, not just putting your own expectations on the individual or family member. I definitely see that a lot. I want this person to get a job and go to school and where they are developmentally with the mental health things going on, that's just not a reasonable or goal, at least at that time it's not an expectation that's realizable.
Speaker 4:Yeah, maybe not realizable at that moment. So I think, being mindful of, is this goal, or is the communication that we are wanting from that individual or person something because we want it, or is this something that can? Is it reasonable? Yeah, that's kind of what.
Speaker 2:I'm thinking about Okay, excellent, thank you. Then I've got one more question, then we're going to ask our listener question. So how can medical professionals, doctors, therapists, caregivers work better together to create a well-rounded support?
Speaker 4:system, I think. Just again back to communication. That's a huge piece. At the job I work at, we meet regularly. We have quarterly clinical meetings, we have check-ins, we have documentation notes that really help us know what's going on. I think, being open to collaborating with folks, especially the medical providers. So we're talking about behavioral health, mental health and physical health. Those go hand in hand. Sometimes, the physical health there's an issue like a UTI or something and it's causing a behavior. So we can't just say, hey, this breathing skill doesn't work. They might just have a medical issue that needs to be addressed. So having everyone on the same page, communicating, is really helpful so we could rule out all the different things that it could be. That's what, yeah, I would say that's a big piece.
Speaker 2:Okay, Any thoughts? Jeff yeah.
Speaker 3:It's something that I feel like when I'm working in combination with a mental health professional on patient care. I really appreciate the insights that the mental health professional gives Because often, even though I try to get to know the person, I can only do so much in 15 minutes, where a person that is in a mental health position often has longer time that they're able to spend with them. So it helps me a lot if something is going wrong, if a medical issue is happening or if there's an adjustment in their mental health medication that's necessary. It's so helpful to have that input and it helps me make better choices and decisions for that patient.
Speaker 4:I agree and I think it goes in all directions. Having the medical input helps the mental health piece, because we could say, okay, this is not a proactive skill, that's going to be helpful because of whatever's happening medically, but also even at the educational or wherever job coaching level, wherever that person is in life, having that communication and being open to hey, this might impact, this is always going to be helpful. I really think.
Speaker 3:Well, and I think also you know if there's a medication change, because almost universally in the population that you're working with, they're on medication Absolutely Okay, and the medication changes can make abrupt and very dramatic changes in a person, whether they could be good or bad. And so understanding from a provider of you know whoever's prescribing the medication, helping know what you might expect as a change or a positive or negative thing, like this particular drug might make your client very sleepy, or this particular medication may make a person wake up more or be irritable, and so having that understanding ahead of time is going to be really helpful for those who are in 24-7 care or even if you're a family member who's watching their ADHD child and change. So, whatever the case may be, staying in good communication with the and understanding how the medications work is a really helpful, important part, I would think things like sleep habits, eating habits, times when they're agitated, times when they're focused and not focused.
Speaker 4:Those are such helpful pieces of information to give to your primary doctor and to share with other people who are maybe adjusting medications.
Speaker 3:It's not only helpful, it's crucial.
Speaker 4:Yes.
Speaker 3:So I love what you just brought up there. Very good, excellent.
Speaker 2:Thank you brought up there Very good, excellent, thank you. Okay, so we're going to go to our question. We've received a powerful question from Jodi, one of our listeners, and this is what she asks as someone with a family member struggling with both a developmental disability and anxiety, I often feel lost in how to support them without overwhelming myself. What advice do you have for caregivers trying to balance their own well-being while providing the best support possible?
Speaker 4:That is a wonderful question and I definitely hear that often. I think the most crucial piece is setting those boundaries, giving yourself time to have your own time self-care. I don't know if there's really one fit all response to how to fix that. However, I think really connecting with like support groups, other family members or people who've been in similar situations. I can't tell you how important it is to reach out to someone who might be in the same situation, because caregiver burnout is huge. It's such a big thing and it impacts people's health so much. I've seen it with caregivers in the agency, but I've also just seen people who have family members. They take care of mental health and physical health issues with their family members and it's a lot.
Speaker 3:In my situation. I see so many. You know it's like a husband that's caring for an Alzheimer's wife or a parent that is the primary caregiver of a disabled, but not completely dependent child. You know where the child can do things, you know, but what they always have is 24-hour, seven days a week on call, so they can never sleep.
Speaker 2:We have a family member like that and they just never, hardly get a break, and it's just exhausting for them about the age of a three or four-year-old at least 22.
Speaker 3:So he can do some things, but he likes to get up in the middle of the night and come into the parents' room and get them up, and you know it's a challenge for them to get any sleep at all, and so it's a very difficult thing for them to get the personal care they need, and especially the mom. The dad often will sleep right through when this happens, but the mom is always up and taking care of it, so she ends up not sleeping well and has put herself in a high alert situation all the time, so she barely sleeps.
Speaker 4:Yeah, I think in those situations we see a lot of caregivers feeling super isolated because of that Cause it's 20, the job is 24, seven, almost like you don't really get a break. It might even be challenging to get that time to talk to someone about it, because it's all day, every day. So I think those support groups I know there's online support groups that have been helpful to folks, but also I see a lot of times people who are caregivers for loved ones or anyone with mental health or physical health, just any kind of caregiver rule that it's hard to see the small victories and the small wins. If you're with someone 24-7, it can just feel like a job it could feel really hard to take a pause. It could be really hard to see that, okay, they're not doing the whole task, but they did one thing more than like. Seeing the little little wins is really, really challenging, I think when you're a caregiver.
Speaker 2:Is there much support for respite?
Speaker 4:care. You know funding changes so often with respite care I don't know a lot are available. I think a good start is looking at DSHS, so Washington State's Department of Health and Human Services website, and looking specifically at the needs. So if it's disability, it would be DDA. I don't know a lot of respites available. Sometimes it's available for youth 18 and under. I see that more common. We used to have respite available for elderly. I don't know what the status of that is, but I think a good start is going to like state websites looking at the National Association of Mental whatever NAMI is. Hold on, I always forget that N-A-M-I.
Speaker 4:N-A-M-I. That website has a lot of caregiver and mental health information and talks about support groups that are local to our area. I know Facebook even places like Facebook have support groups and so those are good places to ask specific questions. Like I have a family member going through this, I'm feeling overwhelmed. What resources are there for respite? I know it changes so often depending on what the funding is and where you're located.
Speaker 3:I can really see how a person in that situation could feel so isolated, and they also feel like no one else can provide the care this person needs better than me or as good as me but I think they also feel that people don't care yeah, yeah.
Speaker 3:and so they get locked into their own cycle of of kind of almost abusing themselves by not getting the self-care that they need. And so I appreciate that you know looking into those things, recognizing that if you're in that situation that you need your own care, you need to be able to take care of yourself, even if it's just taking a break to go to the grocery store by yourself or, you know, seeking out a friend that you haven't chatted with for a while and spending time with them, and recognizing that it's okay, even if it's for an hour, to have somebody else do something for you.
Speaker 4:I agree Absolutely. I think it's so easy to fall in that pattern of feeling hopeless and this is my life and this is all it's going to be, Instead of thinking what can I do to give myself some self-care and it's okay to take a break from this role.
Speaker 2:Excellent. This conversation has been so powerful and I want to thank Nisha Wright for being here with us and sharing her vast knowledge, and for Jodi for sending in that great question. But we're just getting started. In part two, we'll be diving into caregiver burnout, self-care strategies and real-life success stories that highlight the transformative power of behavioral interventions. Make sure you subscribe and you don't want to miss this next episode. And if this episode spoke to you, please share it with someone who needs it. If you have a question, please don't forget to send it to trishajamesoncoaching at gmailcom. And until next time, take care and keep thriving wellness warriors, and we'll see you next time. Bye-bye everyone.
Speaker 3:Bye.
Speaker 2:Bye.
Speaker 1:Thanks for tuning in to the Q&A Files, delighted to share today's gems of wisdom with you. Your questions light up our show, fueling the engaging dialogues that make our community extra special. Keep sending your questions to trishajamesoncoaching at gmailcom. Your curiosity is our compass. Please hit subscribe, spread the word and let's grow the circle of insight and community together. I'm Trisha Jameson, signing off. Stay curious, keep thriving and keep smiling, and I'll catch you on the next episode.










