The Q&A Files
The Q&A Files drops A Wellness Explosion
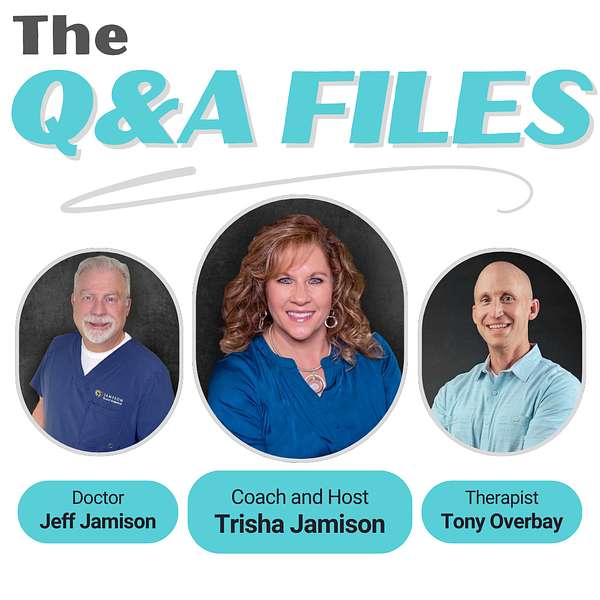
💥 BOOM! Attention Wellness Warriors. The game changer you have been waiting for is finally here. Say hello to “The Q&A Files,” where wellness meets revolution and your questions lead to new discoveries. Spearheaded by Trisha Jamison, your host, a Board Certified Functional Nutritionist. Cohost Dr. Jeff Jamison, a Board Certified Family Physician, and featured guest, Tony Overbay, a Licensed Marriage and Family Therapist. This podcast blends three diverse perspectives to tackle your questions on health, nutrition, medicine, mental wellness, and relationships. Dive into a world of expert insights and actionable advice, all sparked by your curiosity. Tune in, ignite your wellness journey, and join the Wellness Warrior community.
The Q&A Files
57. Caregiver Burnout: Navigating the Stress Loop, with Neesha Wright, Part 2.
Hello and welcome to the Q&A Files, the ultimate health and wellness playground. I'm your host, tricia Jamieson, a board-certified functional nutritionist and lifestyle practitioner, ready to lead you through a world of health discoveries. Here we dive into a tapestry of disease prevention, to nutrition, exercise, mental health and building strong relationships, all spiced with diverse perspectives. It's not just a podcast, it's a celebration of health, packed with insights and a twist of fun. Welcome aboard the Q&A Files, where your questions ignite our vibrant discussions and lead to a brighter you.
Speaker 2:Welcome back Wellness Warriors to part two of our conversation with Nisha Wright. In part one, we laid the foundation for understanding behavioral health and building effective support systems. Today we're diving deeper into caregiver burnout, self-care and the incredible success stories that prove behavioral interventions do work. Credible success stories that prove behavioral interventions do work. Caregiver burnout is a serious issue that affects both physical and mental health. What are the early warning signs that someone is headed toward burnout? First of all, hello, dr Jeff and Nisha.
Speaker 3:Hi everybody. Sorry, I just went right into that.
Speaker 2:We're back here with Nisha so grateful to have her here and we've got Dr Jeff with us, so just curious about what your thoughts are about caregiver burnout.
Speaker 4:I think it's a real thing, it's very common.
Speaker 3:How does it happen? What do you see as kind of the warning signs when a person is getting close to that burnout state?
Speaker 4:I think feeling out of focus, not enjoying what you're doing. So this caregiver burnout is similar to work burnout like feeling like this is overwhelming, not feeling any hope, feeling like your sleep's impacted, like you're always with that caregiver role all the time you stop doing things you love. Very similar to symptoms of depression, where you start losing joy in day-to-day things. Your interest isn't there. Mood changes, dietary changes, easy frustration like your frustration. Tolerance starts to change, maybe feeling more irritable. I think it really looks a lot like a lot of symptoms of depression, unfortunately. Well, that's interesting.
Speaker 3:You know I have a little oil check dipstick level for me that I do in my job that if patients doing normal things start to bother me, it's time for a vacation.
Speaker 4:Oh, that's a good one.
Speaker 3:You know and it's not that I mean I'm really grateful to be in the role I am and I love my patient group. I mean I'm in a great spot where I can basically pick and choose the people that I see and stick with the people that I like and let other people find you know that I don't get along with or whatever to let them go just professionally. But also when you do it for a long period of time, no matter how good it could be, it can get on your nerves, and so I just appreciate what you're saying about the things that can impact a person's behaviors and feelings when you're doing caregiving.
Speaker 4:Absolutely.
Speaker 3:So what do you do, though? What helps you avoid caregiver burnout for yourself? What helps you avoid caregiver burnout for yourself?
Speaker 4:Great question, so it's kind of funny. Some of the skills that I teach with staff or with the individuals I work with are literally the skills that I love using. I spent several years working with kids and teens and there was a lot of mindfulness techniques that we used to practice, and some of the most simplest techniques are the ones that stick with me, such as, like the 5, 4, 3, 2, 1 breathing technique. So demonstrate.
Speaker 3:Tell me what that means? What's the 5, 4, 3, 2, 1 breathing technique?
Speaker 4:So it's more of a mindfulness. You're just paying attention to your breathing. You're looking around, finding five things you see around you.
Speaker 3:And.
Speaker 4:I'm going to do this just because I'm a handsy person, hands-on person when I do it. But I'll look around and spot five things around me. Is there some artwork? There's a lamp, and then there's four things I'm going to feel.
Speaker 4:So, for the folks that like really feel calm with sensory pieces, I'm going to feel the couch, feel my hair, feel this pen over here, and four things, and then hear three things. So I'm going to sit in silence and hear three things. So I could hear my breathing, I could hear the wind outside and I could hear maybe the heater or something, for instance. And then two things, two things I could smell. That one's a little challenging, so you might have to pick up something or find a cup of coffee, smell that or see if there's any smells floating around in the air. And then one thing is going to be, one thing you can taste. So if you have a hard piece of candy or your coffee or drink next to you, you're going to take a sip of that. By the time you get through all those whatever was stressing you out, you're probably not thinking about it because you're putting all your energy focusing on that.
Speaker 2:And I love that. I do that as well, so that is a fantastic.
Speaker 3:One of the things I love about that. Thank you for explaining that too. By the way. I love how that grounds you in now, because a lot of times when we're going through a problem list or we're having these, we're getting stuck in our thoughts and worry. We're not thinking about what's happening right now. We're thinking about how things happened in the past, what bothered us about a past conversation. We're thinking about, oh no, how am I going to deal with not having enough money for this? Or what about my flat tire? You know things, whatever else that you're worried about, how am I going to deal with this next client that just they've been out of control every time I've seen them? And then it can get you out of your head and into the present and ground you into now and that can help you just be so much more ready to deal with the next challenge.
Speaker 2:I love that. Do you have any other techniques that you use?
Speaker 4:I do breathing techniques I really like, just like the basics too. The simpler it is, the easier it is for me to implement that in the middle of my day. So typically a normal office day for me would be I'm working on a report and I'm doing some data mining, trying to figure out patterns of behavior, and then someone will probably come into the office and say, hey, I need you to work on this real quick. And then someone will come in with a crisis and then my on-call phone's going to ring and there's that. And so automatically I'm like how do I prioritize what I'm going to do next? So those five, four, the five four, three, two.
Speaker 4:One grounding skill is one good area. Sometimes I just need to take a deep breath. If that doesn't work, sometimes I'll just take a walk outside. Right now it's cold outside and that's super therapeutic for me, cause I'm like, oh, this is uncomfortable, but it's also taking me out of my mind and helping me slow down. So I like to keep it simple, just because that's another job if I have to think about how to calm myself down or feel better.
Speaker 2:That's so good, so go ahead, jeff.
Speaker 3:I was just going to ask. I know personally things that I feel in my body when I'm feeling stressed. What things do you feel in your body or that you notice other people feel, to be able to help them recognize when stress is getting the best of them?
Speaker 4:So for myself, I notice sometimes my heart rate will go up a little bit, or I just I'm tense, so my muscles are tense and I'll be sitting in my chair just like really.
Speaker 3:With your ears on your shoulders.
Speaker 4:Yes, and I'm like what's going on? And it takes me a minute sometimes to realize I've been sitting this way for who knows how long. So just being able to check in with that, I also noticed, kind of you know, my interactions, my interpersonal interactions are a little bit different. I'm either short with words or like I don't have a lot to say and I'm just ready to be done with the conversation. So that's my instant cue. If I'm at the office and I'm like, okay, I'm done with this conversation and I'm not even present with what the content of the conversation is, if I'm not present in the moment, I think that's a huge piece. I've noticed other people say that they get physical symptoms, headaches, migraines.
Speaker 2:For me, I get a twitch.
Speaker 3:I get an eye twitch or a little facial twitch and if I start feeling that, I know I need to stop, take a couple of deep breaths and just let my shoulders push down towards my hips so that I can take the pressure out of those things and practice those mindful skills that you're talking about. That's just me, so I appreciate the other things that you're talking about.
Speaker 4:I think standing up is also a good one. Just getting out If you're in a sitting position, I think that's huge. Another one I noticed is really not being able to focus on whatever I'm working on. Like it should not be that difficult to continue the task, but if my mind's on something and I can't necessarily pinpoint what it is on my mind and it's just kind of blurry, that's my cue to did I eat? Did I drink water? Did I walk, what's?
Speaker 2:going on Exactly. Do that checkoff list. What do I need to do different?
Speaker 4:Yeah, it might look different for every person, but having that kind of self-check-in, even, maybe even setting a timer on your phone like hey, check-in moment.
Speaker 3:Oh, fantastic, I love that and we're so. When you're working, we're in such a seated position so much of the time. I like that. A lot of places that do office work have sit-to-stand desks. That has really helped, I think, a lot with stress and being able to just detach yourself from your screen every hour or two so that you can look outside and see the environment you're in and get yourself grounded. I love the 5, 4, 3, 2, 1. I'm going to use that and so having those opportunities and I tell people all the time, especially if they bring me problems like their lower extremities are getting swollen or they feel pain in their feet or their legs, but yet they sit all day long and they don't do anything other than sit there looking at a computer screen.
Speaker 2:So they recommend, you know, every hour, to get up and move.
Speaker 3:Right. And I'm one of those people who recommend that.
Speaker 4:I agree. It's also an opportunity to just take a. If you're in an office or work setting, it is that one hour check-in you could walk around and just check in with the environment. Sometimes it's I feel like I lock myself in my office sometimes and I'm there for several hours because I'm focused on like trying to get this data and make sure it makes sense and I forget that like there's a whole world outside of my office Right, yeah, well, that's one thing that I try to do is I'll do like jumping jacks in between clients or something to just get the blood moving through my legs and get the oxygen up to my brain so I can think again.
Speaker 4:I keep a stress ball. I have some of those like stretch bands. So I tried to do like just really simple Like. If it feels like again, if it feels like a workout or a job, I probably won't do it successfully. But if it's just there and I'm like, oh, let me pull this exercise ball right here, let me, like, do some simple exercises, I found that was just super nice If I don't put too much energy into what it is just doing something.
Speaker 3:And it only has to be for a few seconds, I mean you don't have to do it for 15 minutes you just do it for 15 seconds.
Speaker 2:But that time adds up.
Speaker 3:Yeah.
Speaker 2:Yeah, definitely, okay, excellent, thank you. So many caregivers feel guilty when they take time for themselves. How can they shift their mindset to understand that self-care isn't selfish? Now, we've talked a lot about this on our podcast in the past, but I would just like to know what are your self-care things that you like to do for you? Oh, sheesh.
Speaker 4:There's so many Good, Share them. I try to implement it. I mean spending time with my dog. So I have I have two dogs, but my German shepherd is one that's like, she loves hiking and going on adventures. And we live in Washington and it's beautiful, so I take every opportunity I can to spend some time outside walking my dog. That's probably my immediate go-to if I'm stressed, if I'm overwhelmed, if I need to pause walking with my dog, and maybe even going to like Riverside State Park, just checking out places that take me away from my home. So that's my number one. In the summer, kayaking is really peaceful for me. I just I love going kayaking.
Speaker 3:Ooh, that's cool. I love being on the water.
Speaker 4:I remember.
Speaker 2:I used to do that.
Speaker 4:Yeah, so anything water related. I have a friend that has property up in the Green Bluff area and so sometimes I'll sit there overlooking Mount Spokane and sit in a hot tub and read a book or listen to podcasts. I just like how simple it can be. I used to make everything, so I used to be kind of wanting to be a perfectionist and making things so much more complicated than it had to be. I was like I just need to go outside. So I appreciate how simple like the things I love to do Spending time with family. If I feel like I'm losing connection, if I've spent too much time isolating or introverted time, I'll connect with family. But yeah, those are some of the things I love to do. I'm also super crafty and love baking. So anything that has to do with some random craft or baking for other people, I absolutely love doing that.
Speaker 3:Well, and you talked in the last episode about recreating your grandmother's recipe, and that was probably something that really relaxed you and let you feel all the feels for being in the past and in the present.
Speaker 4:It was so much fun. I wish I could show you guys the fail I've now. As I get a little bit older, I find so much joy in the mistakes or the failed experiments of stuff that it doesn't have to be great and perfect the first time, and so things like the recipe not turning out well is hilarious. But maybe in the past that was something that brought me a little more stress.
Speaker 3:So Well, that's awesome.
Speaker 2:Don't you wish that you could take the person that you are now and tell that former younger self hey, stop being such a perfectionist, it's okay to fail, it's okay to do all these things and just, you're going to be great and we just, at the younger age, I don't, I know.
Speaker 3:I appreciate where you're coming from. As always, youth is wasted on the young.
Speaker 4:But I'm grateful I got to the point where I am now.
Speaker 2:So as long as I'm not in that way before.
Speaker 4:I will take that as a total win.
Speaker 2:That's great, Jeff. What are some of your self-care things you do?
Speaker 3:Well in the moment, deep breathing. That helps me a lot Especially. I go from room to room to room to room all day long and after dealing with particularly difficult issues with a patient, sometimes I have to take a minute in between patients I'll just stand in front of the door and take a couple of deep breaths, let my shoulders drop and then say, okay, I can do this, and then open the door and go in the next one. Sometimes I'll stop and go into my office and just take a drink of water, and when I talk all the time as a physician, you can get a little dry mouth, and having something to drink helps me connect with my body a little bit more and help me feel more like I'm getting somewhere. And one of the things that really makes me happy is on my schedule I have little check marks on the next to the names of the patients that I've already seen, and it makes me happy when I've gotten through them and I've got all the check marks done. So I you know I'm a check mark guy and I'm one of those guys that you know if I've got things to do. I like to feel how good it feels to have the check marks done. Now I I don't look at them as those check marks as, oh good, I've treated and streeted these people, that I've worked through my workday, and that's what I'm happy about.
Speaker 3:But over and beyond, I'm a pilot and I love to get in the airplane and go fly, and I love it even more when Tricia can go with me, but I'll go whenever I can. Yeah, and it's fun to just get in the airplane and see the world from a God's eye view and to be able to just and sometimes I just get in the airplane and I just fly around. It's not like I'm flying to anywhere or from anywhere, it's just I just go, fly around the area and look at the beauty of the area. There's lakes and streams and waterfalls and mountains and things all around us, and so just to fly over them and take a look at them is just really relaxing. I can't say grounding, because it's not on the ground, but it is so nice for me and to be.
Speaker 3:I don't know if you've ever felt like this when you were in a car when you were growing up. I don't know if you've ever felt like this when you were in a car when you were growing up, but sometimes when I was in a car growing up, I was a little carsick and I just didn't really like that, and then when I got behind the wheel, I never felt carsick ever again. The same is true when you get in an airplane. If you're sitting in the back looking through the little portholes of an aircraft when you're flying somewhere, you can get airsick. You can, you know, be anxious things like that, and it'd be uncomfortable. But when you're sitting in the front seat and you are the person in charge of the aircraft, all of that stuff goes away, and when you're competent as a pilot, it isn't nerve wracking, it's actually freeing, and so that's one of the things I feel and enjoy.
Speaker 3:That sounds so peaceful, oh, it's wonderful, and I like taking walks with Tricia. We take our dog and we go for a couple mile walk. That's also something that's relaxing for me and I'm learning. I'm trying and I'm learning to love working out in the morning. I'm doing a better job of that, but I've really needed that with the added stress I've had lately.
Speaker 2:Yeah, he's been doing really well with that. That's great, excellent, okay, so let's talk about boundaries. What are some healthy ways caregivers can set boundaries without guilt?
Speaker 4:That's a good, good question.
Speaker 3:She has a lot of those good questions. That one threw me a little off guard.
Speaker 4:I'm like that's like I think the without guilt piece is some of the self-work you have to do on like coming to terms with it's okay to have boundaries. So I think, accepting within yourself, hey, it's okay to have boundaries, and then practice setting them and being okay with it. I think that's maybe a practice kind of piece, Like I don't know if it just magically comes out of anywhere, but I think what helps people find that support and come to the realization that it is okay to have boundaries, nothing's going to go terribly wrong and also we need to take care of ourselves. I think those support groups are just having a community, Whatever that looks like for the person is so important.
Speaker 3:Sorry, nisha, I like to interrupt. I'm sorry about that, but tell me what you would classify as a couple of generic yet very healthy boundaries that are specific.
Speaker 4:I would say, setting the boundaries of, hey, I'm needing to cook my dinner, and saying, hey, I'm not going to take you to the store right now. So I think it's very generic, it's not pinpointed anything. But if someone was really trying to push your boundary, or hey, I want this toy almost like, or I want this item bought for me, and financially that's just not reasonable, instead of giving your all for the thing, saying, hey, this is not something we can do right now, or just setting up the goal. Or just setting up the goal I don't know if it's going to be goal-oriented or what the scenario is for that boundary but being okay, saying no in whatever situation, that is no, we can't go to this place. No, I can't buy this. No, I can't stop what I'm doing right now because I'm working Again, easier said than done.
Speaker 4:It sounds so easy to say, just set a boundary.
Speaker 3:But I know, even until this day I have a hard time and a boundary, but I know, even until this day, I have a hard time, and I always have to check myself and say I think that you said the right thing right there. The key phrase is being able to say no and being okay with it. You know that that is the most simple boundary ever, but it is so profound, so I love what you just said there being able to say no and being okay with it.
Speaker 4:And I could agree. There's no way to get to that point, but it is doable and I think the more you set those boundaries, the more it will be understood and respected.
Speaker 2:Oh, I like that.
Speaker 4:You will get less pushback on the boundary once people know like, hey, you seem serious about this boundary and it's not going to bend.
Speaker 2:And be consistent Excellent.
Speaker 3:I love that.
Speaker 2:Super Okay. So how can caregivers ask for help when they feel overwhelmed? Many struggle with reaching out.
Speaker 4:I think the first piece is identifying that you need help. So no one's going to know if there's an issue or concern or support needed if you can't reach out and say, hey, I need support and I don't know what's going on. A lot of times, I think from the outside perspective, it looks like the caregivers have everything under control and there's no issues. It looks like the caregivers have everything under control and there's no issues. So, unless if that caregiver is like, hey, I'm struggling here, this is playing a toll on my mental health on my day to day. So I think that's a huge first start.
Speaker 4:I hear so often and I've even had family members like people think I'm doing great because I have it under control and I'm taking care of this person and in realistic like, their blood pressure is getting high, their eating's messed up, they're not sleeping well and they're under a lot of stress. So I think, accepting and understanding, hey, I am in a stressful situation and being able to talk to someone about it, whoever that person is, in hopes that that person will be able to say, hey, have you tried this? And, if not, keep talking. I don't think it's something. Do not invalidate your own experience of what you're going through and thinking that people aren't going to understand or not want to hear it.
Speaker 3:Okay, don't invalidate your own experience. Yeah, I love that.
Speaker 4:We talk about validating other people's experiences, but do we validate our own experience? Like we just brush it aside and we focus on the other person, and it's sometimes hard to just take a pause and be like, oh wait, did I just brush off my own experience as not as big of an important.
Speaker 2:Yeah, oh, I think that's so good. So good, okay. So what role does community support play in avoiding burnout? We've kind of been talking about burnout, but I wanted to ask this question and where can caregivers find resources?
Speaker 4:So in the supported living situation a lot of times agencies have they already know caregiver burnout's a huge piece. So there's a lot of tools built in, whether it's calming rooms, online virtual rooms, trainings on support and a lot of resources and if you're in an employment type setting, you have, like your EAP and kind of supportive resources.
Speaker 2:What does EAP mean?
Speaker 4:Employment Assistant Program. So a lot of jobs have those built into and they'll have like counseling and a lot of things that resources for caregivers.
Speaker 3:So one of the things that do you find that when people are reaching out, that some people don't fit the needs of the person that's having the crisis moment. So if you go into a counseling situation and you don't feel safe, you don't have a connection, you don't feel heard even though't have a connection. You don't feel heard even though validation is such a big part of counseling. If you don't feel like you're connecting with your counselor or a person that you're trying to connect with, then that's the wrong person 100% agree on that and I think it's important for people when I say don't you know?
Speaker 4:don't stop talking to people about your experience. Also, don't give up on the process. When I meet with folks for individual counseling, I'm like you know we might not be the right fit, it's okay, it's so okay if we're not the right fit for each other, because someone is the right fit for you, but it's not a. You know, there's not one therapist who's going to be perfect for every single person, or one counselor or one support network.
Speaker 4:So I think it's super important to just go out there, and it might take a little bit of homework at first, but when you're with the right people, the right resources just really are there, and if they're not, there's the right community of people who understand that the resources aren't available that you need.
Speaker 3:And that at least helps the isolation piece.
Speaker 3:Oh, that's so helpful and I feel like there are so many maybe occupation-specific people to talk with. There's situation-specific people, like people that have a person at home that needs 24-7 care, People that have a person at home that needs 24-7 care. That's a specific group of caregivers that they can relate to each other really well, but if you're not talking to somebody in that situation, they wouldn't really be able to offer you any kind of support. Finding your people is such an important part of this of the process of improvement of your self-burnout, of your burnout. Am I on the right track on that?
Speaker 4:I absolutely agree. Definitely don't give up on that process. I'm not a huge fan of social media, but one thing that is a strength of social media is that sometimes it connects support groups. That is a strength of social media is that sometimes it connects support groups online when it's not accessible in person or due to your time constraints or work or whatever it is you're doing. And so if in person isn't possible or you can't find your people, definitely reach out to different support groups. You will find someone who will be able to direct you in the right place. Or you might just find your group, and I just think it's priceless to be able to direct you in the right place. Or you might just find your group, and I just think it's priceless to be able to have someone who understands what you're going through and can be unjudgmental, and there and everyone needs that.
Speaker 4:I mean, that goes way beyond caregiver, burnout and just in general.
Speaker 2:Yeah, oh, thank you. That's so great. All right, so, nisha, you've worked with so many families. Can you share a success story that really stands out, one where a behavior plan made a huge impact?
Speaker 4:Okay. So right now I'm working with primarily individuals in supported living agency and right now I'm actually currently working on a plan where this person has more independence in the community. And so what it looked like was when I first started working with this individual not directly all the time, because I'm doing like the behind the scenes plan writing, teaching the staff but they had a lot of restrictions, their sharps were restricted, they couldn't be alone in the community. They had two staff. Over time this person joined our Green Zone. So my agency has a program called Green Zone but it's kind of like mindfulness DBT. There's a lot of skills taken from different modalities to adapt to the agency and this individual. She went through the whole program, graduated from the program and at the end of that one was able to know enough skills to even teach some of the calming skills and how to get through it. But also a lot of her restrictions were reduced and we're now on the point where she could go to the grocery store and practice doing most of the shopping by herself.
Speaker 4:And this is a person with at one point was hospitalized at Eastern, had extreme behaviors, also developmental disability, and now we're in a place where I mean, they've come a long way and it's just such a beautiful thing to see. And the behavior plans are what fuel practicing those skills. So without that behavior plan in place they wouldn't know what green zone skills or mindfulness skills to work with. And it definitely took a lot of time practicing those skills. But you get to see the strength and ability a person has. I think we get stuck thinking some people can't change or we don't see change fast enough, so it doesn't seem like change is happening at all. So it's really great to have those little moments where you could see someone actually make a drastic change, even if it took two to three to four years.
Speaker 2:Right.
Speaker 3:Yeah, so yeah, I mean just as a point of clarification to you mentioned that she was hospitalized at Eastern and I wanted to put a little exclamation mark on what that means. When a person is hospitalized at Eastern State Hospital, that's a locked mental health unit and that is a place where sometimes criminally and dangerously mentally ill people reside with 24-7 surveillance. So in order for a person to understand how incredibly sick this person was that Lisa's talking about, that's the situation she was in at Eastern State Hospital.
Speaker 4:Absolutely, and it's amazing to see the growth. I wasn't there for the whole process, but I've got to see the growth over time and now I work with this person every single week. We meet and check in and just it's unbelievable. Like it's not perfect, there's still you know, times where emotions get dysregulated. But how old is she? She is 24, 24 now.
Speaker 2:Okay, okay, wow. Well, that sounds like she's been in since 18.
Speaker 4:So she started supported living, I think at 18 or 19, and with belts of Eastern and for state station.
Speaker 2:And that was helpful for her.
Speaker 4:It was.
Speaker 2:Okay.
Speaker 4:I mean it took so long to get to that point. So I think the reason I share that is because for the folks who are with the individual they're helping out or who the caregivers you're with them every day, 24, seven, it's really hard to see the little change and see the big picture that, like something big like this can happen. I'm sure the staff providing services when she first started supported living did not see that she would be where she is today.
Speaker 2:Wow.
Speaker 3:That's great. It's glad to see progress.
Speaker 2:Yeah, that's great. Thank you for sharing that. So if you could change one thing about society and how they support individuals with disabilities, what would it be?
Speaker 4:I would just say the communication around it, the understanding that I would just say the education and communication about it. I think a lot of people make up their own idea of what they think a person with disability can and can't do.
Speaker 2:Because I think people are fearful.
Speaker 4:Yeah, and I think just having more education available about it, having more platforms where people can ask questions and challenge what their judgments or thoughts are, what people told them about it, I think that's a good start. I think just the knowledge piece of it.
Speaker 2:Excellent, fantastic.
Speaker 3:I think it's really easy to kind of group or lump everyone that has a mental disability or a mental illness into a group of those people you know and instead of recognize they're all individuals with strengths and value, and that's the thing that I think is a really hard one to have the population at large have compassion for us to value.
Speaker 4:And I think just the stigma around people with disabilities or mental health, like reducing that and also knowing that there's a whole spectrum of like what that looks like mental health illness there's day to day. I mean, there's a lot of people you don't know have mental health illness or maybe a developmental disability and they're functioning just fine. So, it's really the assumption that breaking that stigma, or assumption that if you have a mental health illness or a disability, that you can't function and do the day-to-day things that everyone else does.
Speaker 2:Yep so yeah, excellent, so good. So is there any final insight or advice that you would like to leave our listeners with today?
Speaker 4:I would just say, caregiver or not, the self-care piece is so important. The older I get, the more I realize like, hey, I do like using these skills and I remember a time teaching them to like kiddos and they're like oh, this is stupid, I don't like this skill. And then you see them using the skill and they're like oh, I feel better and now I'm doing that for myself regularly and just remembering to take care of yourself. Like I think that answers all the questions we've talked about. Like if we're not able to be there for ourselves, we can't be there for other people. It's really going to be hard to help someone if we can't make sure we're taking care of ourselves.
Speaker 3:Wonderful. I love that being self-aware and then taking care of yourself so good.
Speaker 4:The best that you can with what you're working with.
Speaker 3:Right and you can't use tools you don't have. So seek out tools and seek out people that know more than you, so that you can get better on an ongoing basis.
Speaker 2:So yeah, I love that. Seek out people that know more than you Very good.
Speaker 3:Yeah.
Speaker 4:I love that idea too. I love learning, so like it comes natural to me and I forget sometimes that some people don't naturally want to reach out and do those things. So I think that's a great tip for folks.
Speaker 2:Sounds great, jeff, do you have any other last minute remarks? You'd like to make.
Speaker 3:Just a plug for something that's coming up for us. I think that it's important to know that we find this incredibly important to have self-care and help you understand your own limitations and your own needs, and there's specific care that is needed by people that understand medicine. If you're a doctor, for instance, and you are in a relationship with your spouse, that is sometimes difficult because of the balance that happens between your career and your family, and Tricia and I are developing a new program to help physicians and spouses improve their relationships so that they don't run into some huge problems that can happen in these very specific relationships. So this is one of those developing communities that we're working on right now to be able to give back to a community that has helped us, and we are looking forward to it.
Speaker 2:We are, and when we were putting things together, it was what are all the things that we wish that we had going through training and early marriage, medical marriage and we hope that this will be able to reach many, many medical families out there that are struggling. Nisha, thank you so much for joining us. This was so great. It was just so fun to have you on. Great to see you. You're beautiful.
Speaker 2:Thank you, yes, and we also want to thank our listeners, and if today's episode resonated with you, please remember you're not alone and please remember that there's help out there. We're there to help you, we're there to help you and there's resources to help you as well. We will make sure that we'll put things in the show notes that Nisha has suggested for you. She was just a wealth of information and we're so grateful that she was here with us. If you have a burning question or if you need a health coach to help you navigate life's challenges, I'd love to help you create a plan that works for you as well. So reach out anytime at Trisha Jameson coaching at gmailcom, and until next time, take care and keep thriving wellness warriors. See you next time. Thank you, bye-bye.
Speaker 1:Bye. Thanks for tuning into the Q&A Files, delighted to share today's gems of wisdom with you. Your questions light up our show, fueling the engaging dialogues that make our community extra special. Keep sending your questions to trishajamesoncoaching at gmailcom. Your curiosity is our compass. Please hit, subscribe, spread the word and let's grow the circle of insight and community together. I'm Trisha Jameson, signing off. Stay curious, keep thriving and keep smiling, and I'll catch you on the next episode.










